Root canal treatment is a dental procedure aimed at treating the infection at the centre of a tooth, the pulp, which contains nerves and blood vessels. Root canal treatment involves removing the infected or damaged pulp, cleaning and disinfecting the area, and filling and sealing the tooth. The primary goal of root canal treatment is to save and restore a tooth that is severely decayed or infected, preventing the need for extraction.
The importance of root canal treatment is to prevent infection in the pulp that causes an abscess or spreads into the jawbone and surrounding tissue if left untreated, leading to severe pain, bone loss, and general health complications. A root canal helps treat the infection and save the natural tooth. Root canal treatment helps preserve oral health and reduces the need for more complex and costly treatments in the future.
 A general dentist or an endodontist performs root canal treatments. An endodontist is a dentist who specialises in treating diseases and injuries of the dental pulp, or the root of the tooth. Endodontists have additional years of training specifically focused on performing root canal therapy and other procedures relating to the interior of the tooth.
A general dentist or an endodontist performs root canal treatments. An endodontist is a dentist who specialises in treating diseases and injuries of the dental pulp, or the root of the tooth. Endodontists have additional years of training specifically focused on performing root canal therapy and other procedures relating to the interior of the tooth.
The primary benefit is the preservation of the natural tooth, which allows for normal biting force and sensation and maintains the natural appearance of the tooth. Root canal treatment helps protect the other teeth from excessive wear or strain.
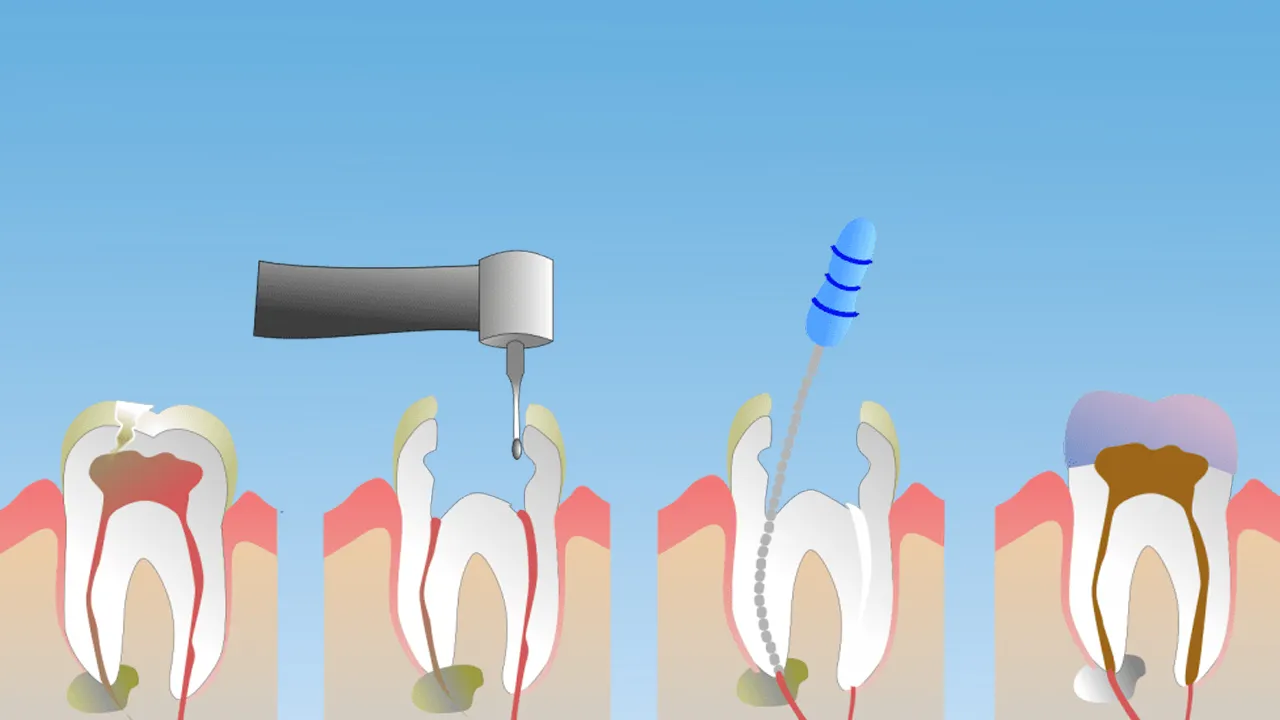
The root canal procedure is usually performed in three primary steps such as cleaning the root canal, filling the root canal and adding a crown or filling. The cleaning process involves creating an access hole on the surface of the tooth and removing the damaged or diseased pulp. The dentist fills in the canal with a material called gutta-percha after the root canal is cleaned, which helps to keep the canals free of infection or contamination. The final step is restoring the tooth with a crown or filling for protection. The step is essential because it prevents the tooth from cracking and ultimately failing if the procedure is not completed.
Root canal recovery time takes a few days for most patients. It varies depending on the difficulty of the operation and the patient's individual circumstances. Post-operative symptoms usually include mild pain and discomfort, which are managed with over-the-counter pain medications. Patients expect to return to normal oral function after the recovery period
1. Examination with X-Rays
Examination with X-rays is a crucial initial step in the procedure for dental root canal treatments. It takes radiographic images of the patient's teeth and jaws to gain a comprehensive view of the affected tooth and the surrounding bone structure. X-rays allow the dentist to clearly see the interior aspects of the teeth and gums that aren’t visible to the naked eye.
The importance of the procedure lies in the valuable information it provides. X-rays reveal the shape and size of the root canals and the extent of the decay or infection. It allows the dentist to identify any signs of an abscess, bone loss, or other abnormalities in the surrounding bone structures. X-rays offer a roadmap to the dentist, guiding them in their treatment plan.
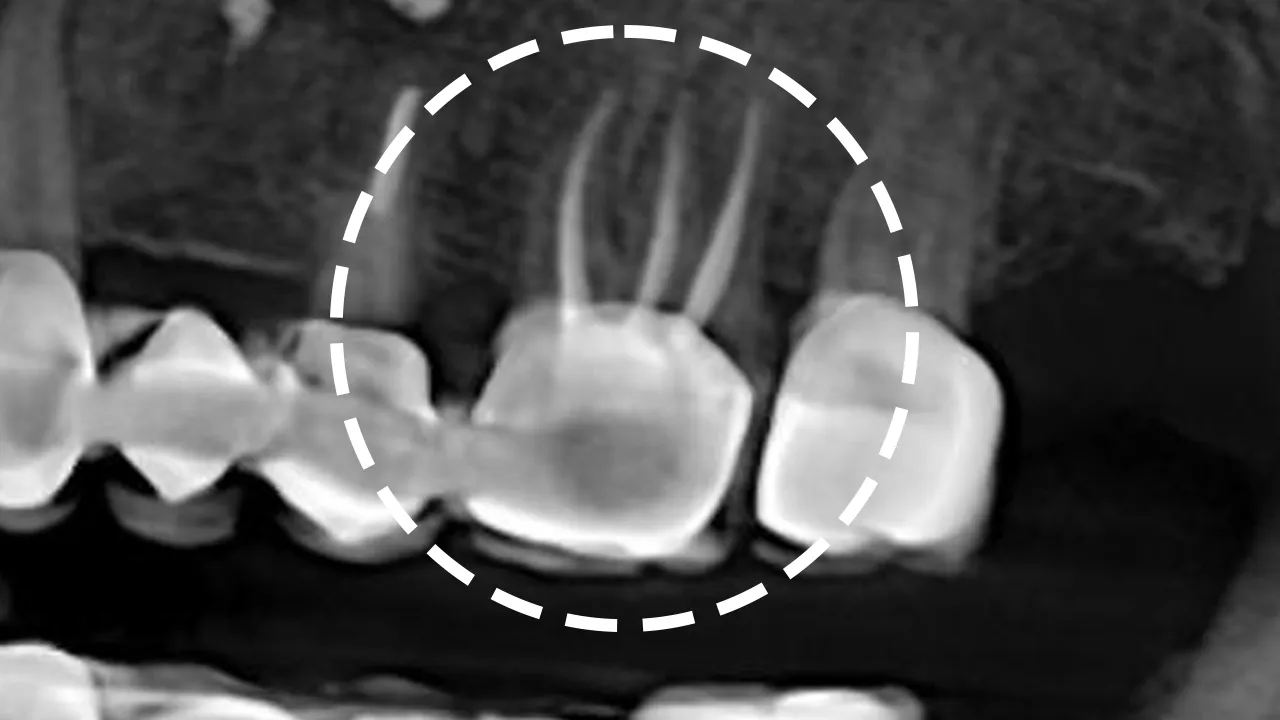 The necessity of an examination with X-rays for the next steps in the procedure is vital. Data obtained from the X-rays determines how the dentist approaches the root canal treatment. Knowing the number of roots and the shape of the canals helps the dentist accurately remove all the infected tissue from the tooth. It highlights any additional canals that aren’t present or any unusual anatomy that requires a different treatment approach.
The necessity of an examination with X-rays for the next steps in the procedure is vital. Data obtained from the X-rays determines how the dentist approaches the root canal treatment. Knowing the number of roots and the shape of the canals helps the dentist accurately remove all the infected tissue from the tooth. It highlights any additional canals that aren’t present or any unusual anatomy that requires a different treatment approach.
X-rays are taken during the procedure to help ensure that the cleaning and shaping of the canals are done effectively and that the filling material adequately seals the entirety of the canal. Post-procedure X-rays are necessary to assess the success of the treatment and monitor healing during follow-up visits. Examination with X-rays is an essential part of the root canal procedure, from initial diagnosis and planning to execution and follow-up. The likelihood of a successful root canal treatment greatly drops without X-rays.
2. Local Anaesthesia
Local anaesthesia is a type of medication used in root canal treatments to numb a specific area of the mouth. The purpose of local anaesthesia is to block nerve signals in the body, numbing the sensation in a particular area, and allowing dental procedures to be carried out without pain or discomfort. It is usually administered through an injection directly into the tissue near the tooth to be treated.
The importance of local anaesthesia in the procedure for dental root canal treatments is important. Root canal treatments involve working with very sensitive nerve tissue that causes a lot of pain if it isn’t numbed first. The use of local anaesthesia ensures that the patient undergoes the procedure comfortably and without distress. It promotes patient cooperation, as a calm and relaxed patient makes the dentist's work easier and more accurate.
The necessity of local anaesthesia for the next steps in the procedure is critical. The dentist proceeds with the actual root canal treatment once the patient is adequately anaesthetised. It involves drilling a small hole into the tooth and removing the infected or inflamed pulp tissue. The steps are excruciating without proper anaesthesia, and the patient's instinctive reaction complicates the procedure.
The dentist cleans, shapes, and fills the root canal after removing the infected pulp. Each of the steps stimulates the nerves in the area, causing discomfort or pain if not for the effect of the local anaesthesia. Local anaesthesia ensures that the process is painless and as comfortable as possible for the patient from the start of the procedure to its completion. Performing a root canal treatment is challenging for the dentist and the patient without local anaesthesia.

3. Placement of A Dental Dam
The placement of a dental dam is another vital step in the method for dental root canal treatment. A dental dam is a very thin and flexible sheet of latex or non-latex material that isolates the tooth being treated. The dam sits over the affected tooth, allowing just the tooth being treated to be exposed while the rest of the mouth is covered and protected.
Dental dams are important as they reduce the risk of infection by preventing bacteria in the saliva from entering the tooth once the root canal has been opened. Protecting the patient's mouth by preventing the ingestion or inhalation of dental instruments, irrigants, or debris from the tooth during the procedure. The dental dam provides a clean and dry working area for the dentist, making the operation more efficient and straightforward.
The necessity of placing a dental dam for the next steps in the procedure is crucial. The subsequent steps in a root canal procedure involve the use of small instruments and chemicals that harm the patient's mouth if not isolated correctly. The dental dam acts as a safety measure, protecting the other areas of the mouth from exposure to tools and substances.
The dentist safely and effectively cleans the infected pulp after the dental dam is in place in the root canal, fills the canal with a biocompatible material, and seals the tooth. Confident that the patient's mouth is well-protected and the tooth that's being treated is as free from bacteria as possible. There is a higher chance of injury, infection, and complications during a root canal procedure without the placement of a dental dam. The dental dam is a critical component of a proper and effective root canal procedure.
4. Access to The Pulp Chamber
The pulp chamber is a space within the tooth that houses the pulp. Pulp is the soft tissue consisting of nerves and blood vessels. The dentist drills a small hole into the tooth, specifically into the crown for molars and premolars and the back of the tooth for front teeth, accessing the chamber.
The importance of gaining access to the pulp chamber during root canal procedures is crucial. The primary reason for it is that the infected or inflamed pulp that is causing the patient's pain or discomfort resides within the chamber and the connected root canals. The dentist must gain access, clean, and disinfect the area to treat the infection and alleviate the patient's symptoms.
The necessity of accessing the pulp chamber for the next steps in the procedure is absolute. The Dentist removes the infected or inflamed pulp tissue once the dentist has access to the pulp chamber, effectively eliminating the source of the tooth's problem. The dentist cleans and disinfects the pulp chamber and root canals following the removal of the pulp, a process known as irrigation. The cleaned and disinfected pulp chamber and root canals are filled with a biocompatible material to seal the tooth, preventing further infection.
5. Removal of Infected or Damaged Pulp
Crucial to any root canal surgery is the extraction of diseased or otherwise damaged pulp. The pulp contains the tooth's blood vessels, nerves, and connective tissue. Pain, swelling, and an abscess or systemic infection arise if the person ignores the symptoms of pulp damage or infection caused by extensive decay, several dental operations, defective crowns, or a cracked tooth. Special dental instruments are used to clean out the pulp chamber and root canal of the tooth in order to remove the infected or damaged pulp.
The removal of infected or damaged pulp is crucial to the outcome of a root canal operation. Removing the infected or inflamed tissue reduces pain and swelling, stops the development of infection, and saves the tooth and its surrounding tissues from further harm. It lays the groundwork for the succeeding stages of treatment, such as cleaning, disinfecting, and filling, which are necessary for the tooth's recovery and preservation.
The next procedure requires the removal of infected or damaged pulp. The root canals and pulp chamber are later cleaned and disinfected by the dentist. Steps taken to clean and disinfect thoroughly are essential for preventing a recurrence of an infection. The tooth's pulp chamber and root canals are sterilised, cleansed, and filled with biocompatible material to prevent reinfection.
The problem remains unfixed if the contaminated or damaged pulp is not removed and the next steps of clean-up, disinfecting, and filling result in failure. The step is critical to restoring the tooth's health and functionality and ensuring the lasting efficacy of the root canal treatment.
6. Irrigation
Root canal treatments in dentistry rely heavily on irrigation. The dentist flushes the pulp chamber and root canals with a disinfecting solution, such as sodium hypochlorite or chlorhexidine after the infected or damaged pulp has been removed. The solution aids in the removal of any lingering bacteria, the dissolution of pulp tissue, and the thorough cleaning of the canals.
Irrigation is crucial to the success of root canal procedures for many reasons. Root canals are disinfected to lessen the likelihood of reinfection. Irrigation with a disinfectant solution reaches crevices in the root canal system that traditional cleaning equipment misses. Improving the quality of cleaning in every way possible. The filling and closing parts of the treatment happen in a clean environment made possible by irrigation, which helps drain away debris, dead tissue, and germs.
The next steps in the root canal procedure require irrigation. The dentist proceeds to fill and seal it once the root canals are thoroughly cleaned and disinfected through irrigation. Filling and sealing the root canals serves to prevent future bacterial contamination, but if the canals aren't properly irrigated and contain bacterial remnants, the risk of post-treatment infection remains high.
Filling and sealing over canals that haven't been adequately cleaned traps bacteria inside, which defeats the purpose of the treatment. The irrigation phase is a vital link between the initial cleaning phase and the final sealing phase of a root canal treatment. Ensuring the optimal cleanliness and sterility of the root canals before they are permanently sealed. The effectiveness and long-term success of root canal treatment are severely compromised without thorough irrigation.
7. Filling the Canals with Gutta-Percha
Filling the canals with gutta-percha is a decisive stage in the procedure for dental root canal treatments. Gutta-percha is a rubber-like material derived from the sap of the Malaysian gutta-percha tree. The pulp chamber and root canals have been thoroughly cleaned and disinfected during the irrigation phase and filled with gutta-percha. The gutta-percha is heated and compressed into the canal, and a sealer is used to fill any tiny spaces between the gutta-percha and the canal walls.
Filling the canals with gutta-percha is a crucial step in root canal treatment. The main objective of gutta-percha is to provide a stable, inert filling for the now-empty pulp chamber and root canals. Gutta-percha helps prevent reinfection by blocking the pathways that bacteria use to reenter the tooth by filling and sealing the spaces. It’s well-tolerated by the body because gutta-percha is biocompatible, ensuring that the tooth continues to function without causing discomfort or adverse reactions.
Gutta-percha is needed to fill the canals for the next steps. The dentist proceeds to restore the tooth with a crown, providing strength and protection once the canals are filled with gutta-percha. The tooth remains hollow and susceptible to further infection or structural damage without filling the canals with gutta-percha. The filling helps maintain the tooth's integrity and prevents it from breaking.
There is a void space within the tooth that harbours residual bacteria or becomes recontaminated over time if the canals aren’t filled. Filling the canals with gutta-percha is a vital step in root canal treatment that bridges the gap between the initial cleaning and the final restoration of the tooth. Ensuring the tooth's long-term health and stability.
8. Placement of A Temporary Filling
The dental root canal procedure begins with a temporary filling. The dentist places a temporary filling in the access hole created to enter the pulp chamber, following the filling of the canals with gutta-percha. The temporary filling serves to seal the tooth, protecting it from contamination from food particles, bacteria, and saliva until the permanent restoration is completed.
The temporary filling in root canal treatments is crucial to maintaining the cleanliness and sterility of the work done so far by preventing oral bacterial invasion. Providing an immediate seal on the tooth reduces the likelihood of pain or discomfort that otherwise occurs from exposed nerve endings.
The necessity of placing a temporary filling for the next step in the procedure, which is the placement of a permanent restoration, is equally significant. The time interval between the root canal treatment and the placement of a permanent restoration leaves the tooth vulnerable to recontamination. The tooth is structurally weakened and more susceptible to damage from the forces of biting and chewing without a temporary filling.
The placement of a temporary filling acts as a protective measure that helps to maintain the sterility and integrity of the tooth during the time before a permanent restoration is done. Ensuring that the groundwork laid by the cleaning, disinfection, and filling of the canals is not compromised while the patient awaits the final step of the procedure. The treatment fails due to recontamination or structural damage without it.
9. Crown Placement
Crown placement concludes dental root canal treatments. A dental crown is placed on the treated tooth after the pulp chamber, root canals, and temporary filling are cleaned, disinfected, and filled. The dental crown is made of porcelain or metal, custom-made to fit over the tooth and copy its natural figure, size, and colour. Providing an extra layer of durability and protection effectively shields the tooth from future damage and ensures its functionality in the long term.
Crown placement is a very important part of root canal treatment. Root canal treatments leave the treated tooth weakened and more prone to fracture. It is due to the removal of the tooth's pulp and the consequent reduction in the tooth's blood supply and nutrition. Placing a crown after a root canal treatment provides the necessary reinforcement to the tooth, helping it withstand the forces of biting and chewing. It allows patients to use their teeth naturally without fear of causing damage.
The necessity of crown placement for the longevity of the treated tooth remains vulnerable to fractures and breaks under the strains of normal use. The temporary filling that was placed after the root canal treatment to seal the tooth isn’t designed to withstand prolonged exposure to the oral environment. The crown provides a durable and long-term seal that protects the tooth from reinfection and helps ensure the success of the root canal treatment.
The crown placement is the final yet critical step in root canal treatment. The crown completes the restoration of the tooth, helping it to regain its strength, functionality, and appearance, ensuring the long-term health of the tooth post-procedure. The risk of tooth reinfection compromises root canal treatment without a crown.
What is Root Canal Treatment?
Root canal treatment is a way to save a badly decayed or infected tooth through a dental procedure. The treatment involves the removal of the inflamed or infected pulp, the innermost part of the tooth containing blood vessels, nerves, and connective tissue, cleaning and disinfecting the interior of the tooth, and filling and sealing it. The term root canal comes from the cleaning of the canals inside the tooth's roots.
A deep cavity that has allowed bacteria to reach the pulp is what causes a root canal procedure, leading to infection and inflammation. Damage or trauma to a tooth, such as a crack or chip, exposes the pulp, making it vulnerable to bacterial infection. Dental root canal procedures performed on the same tooth multiple times lead to the need for a root canal due to repeated exposure and potential damage to the pulp.
The process of a root canal treatment seems daunting, but it is a necessary measure to relieve pain and save the tooth from extraction. The benefits of saving the natural tooth with a root canal include efficient chewing, normal biting force and sensation, and the maintenance of a natural appearance. Root canal treatment helps protect the other teeth from excessive wear or strain.
The process seems long and scary but advances in modern dentistry, such as better anaesthesia and more precise tools, make a root canal as comfortable as getting a filling. The procedure is a tooth-saving treatment, offering an opportunity to maintain natural tooth and oral health for many years. A tooth treated with a root canal lasts a lifetime with good oral hygiene and regular dental check-ups.
How Important is the Root Canal Treatment?
Root canal treatment is important because it saves a badly damaged or infected tooth that has to be taken out. Root canal treatment gets rid of pain and stops an infection from getting worse by removing the infected or swollen pulp, cleaning and cleansing the inside of the tooth, and closing it. The treatment stops the infection from spreading to other teeth and the bone structure around them, which causes more problems.
The advantage of root canal treatment is its ability to save the natural tooth. Preserving a natural tooth helps maintain the functionality and aesthetic appearance of the patient's mouth. Ensuring efficient chewing allows for normal biting force and sensation and reduces the need for more complicated and costly tooth replacement treatments. The loss of a natural tooth leads to other oral health problems, such as difficulty chewing and the shifting of other teeth, which result in a misaligned bite.
Root canal treatment prepares for other dental procedures by creating a stable base for further restorative treatments. The crown is placed on the tooth to strengthen it and restore its shape and function once the root canal treatment has been successfully done. The root canal treatment forms a base for the crown placement, saving the tooth from extraction and ensuring a robust and durable fix.
Who Performs the Root Canal Treatments?
Root canal treatments are done by both endodontists and general dentists. The general dentist is the primary dentist who examines, treats and takes care of oral health needs, such as gum care, root canals, fillings, crowns, veneers, bridges, prevention education, and more. Root canal treatments are something that most general dentists are familiar with and are able to perform, especially if the process is simple and the tooth isn't complicated.
Endodontists are dentists who solely diagnose and treat tooth pain. They perform root canals and other procedures that deal with the inside of the tooth. Endodontists get an extra two to three years of training after dentistry school, which focuses on the kinds of treatments they do. The advanced training and specialised techniques allow them to handle more complex root canal cases, such as those involving severe infections, multi-rooted or confined canals, or the re-treatment of previously unsuccessful root canal procedures.
An endodontist is recommended for more complex cases or if complications arise while general dentists perform root canal treatments. Professionals are integral parts of the dental field and work together to ensure that patients receive the most effective care for their specific needs. The decision about whom to perform a root canal treatment depends on the complexity of the tooth's structure, the extent of the problem, and the comfort level and experience of the general dentist with the procedure.
Why is Root Canal a Type of Common Dental Procedure?
Root canal treatment is a common dental method for most patients who require it because it is effective in treating a variety of dental issues. The potential of root canal operations to save and restore teeth at risk of being extracted is the fundamental rationale for the widespread use of these procedures. Infection or damage to the tooth pulp, which comprises nerves, blood vessels, and connective tissue, causes significant pain and leads to the formation of abscesses as a result of deep decay, trauma, or repetitive dental operations. The infected or inflammatory pulp from the inner chamber and canals of the tooth is removed during the root canal operation, after which the area is disinfected, filled, and sealed to prevent further infection. The process of performing a root canal saves the natural tooth, allowing the patient to keep their normal biting, chewing, and speaking abilities.
The data provided by dentists and researchers supports the widespread use of root canal procedures. The American Association of Endodontists estimates that dentists in the United States alone perform millions of root canal procedures each year. The excellent success rate of the surgery, as well as its long-term usefulness in relieving pain and saving teeth, have contributed to its widespread adoption. Numerous research studies have shown that root canal therapy is successful, with success rates ranging from 85 to 97% after a ten-year follow-up period. The studies have shown results.
Root canal procedures are considered a preparatory step for more extensive dental treatments such as crown and bridge work. It is crucial to ensure the health and stability of a tooth before restoring it with the appropriate . types of dental crown or bridge. It is vital, prior to the placement of these restorations, to make sure that the pulp and nerves of the tooth are in good health. Dental restorations are not going to be as effective or last as long if the pulp is diseased or damaged. A root canal procedure performed before any restorative work is done ensures that the tooth is healthy and free of infection, providing a solid base for the work that follows.
Root canal procedures are frequently performed in dentistry because of their capacity to prevent the loss of teeth and restore the teeth's capacity to function normally. The method receives backing from the evidence that demonstrates its high success rates and effectiveness over the long run. Root canal procedures function as preparatory procedures for other significant dental treatments, assuring the tooth's health and stability prior to restorative work being performed on it.
What are the Benefits of Root Canal Treatments?
The benefits of root canal treatments are listed below.
- Pain Relief: Pain relief is one of the main perks of getting a root canal. The procedure addresses the source of severe toothache caused by infected or damaged pulp (inner tissue of the tooth), providing quick and effective pain alleviation.
- Preservation of Natural Teeth: Root canal treatments aim to preserve the natural teeth. The dentist preserves the tooth's form and functionality by taking out the infected pulp and cleaning the inner chambers of the tooth.
- Prevention of Infection Spread: Infected dental pulp leads to abscesses or infections, which spread to other areas of the mouth and even the body if left untreated. A root canal halts the spread of infection, preventing more serious health complications.
- Improved Oral Health: A root canal contributes to maintaining oral health by eliminating infection and saving the natural tooth. Preserving the tooth's integrity ensures proper chewing function and prevents neighbouring teeth from shifting.
- Natural Appearance: Root canal-treated teeth retain their natural appearance, ensuring a seamless smile. A dental crown is placed to restore both aesthetics and functionality after the procedure.
- Efficient Chewing: A tooth treated with a root canal and crowned functions effectively, allowing the patient to chew and bite comfortably. Helping maintain a well-balanced diet and supporting proper digestion
- Cost-Effective Solution: Root canal treatment is frequently more affordable than tooth extraction and replacement options such as dental bridges or implants. It addresses the issue directly while preserving the natural tooth.
- Quick Procedure: Modern root canal treatments are relatively quick and efficient. The procedure is completed in a single visit, saving time and minimising the need for multiple appointments.
- Minimal Discomfort: Root canal treatments are performed using local anaesthesia, ensuring minimal discomfort during the procedure. Advances in dental techniques have improved patient comfort during and after treatment.
- Longevity: A tooth that has undergone a root canal treatment lasts a lifetime when properly cared for. Regular dental check-ups and good oral hygiene practise help maintain the restored tooth's health.
- Avoidance of Extraction: Root canal treatments offer a viable alternative to tooth removal. Keeping a natural tooth helps maintain the bone structure in the patient's jaw and prevents the potential complications associated with tooth loss.
- Restoration of Confidence: The relief from pain and the restoration of a healthy smile boost the patient’s self-confidence, allowing them to interact with others without the discomfort or self-consciousness caused by dental issues.
What are the Limitations of Root Canal Treatments?
The limitations of root canal treatments are listed below.
- Fractured Roots: A tooth's roots are severely fractured or damaged in some cases, making it difficult to effectively clean and seal during a root canal procedure. Leading to extraction instead.
- Severe Decay: A root canal isn’t sufficient to save the tooth if the tooth decay is extensive and affects a significant portion of the tooth structure. The remaining decayed tooth structure isn’t strong enough to support the restoration.
- Limited Access: The anatomy of certain teeth makes it challenging to access and thoroughly clean the complex root canal system. The limitations compromise the success of the procedure.
- Incurable Infections: An infection is resistant to treatment or located in an area that's difficult to reach and effectively clean in some cases. Resulting in the need for tooth extraction.
- Weak Tooth Structure: Teeth that have undergone multiple dental procedures or have extensive damage weaken the structures. A root canal-treated tooth with compromised strength is prone to fractures, necessitating additional restoration or extraction.
- Pre-existing Structural Issues: Teeth with significant structural problems, such as large fractures or insufficient tooth material for restoration, aren’t ideal candidates for root canal treatment.
- Post-Treatment Discomfort: Modern techniques aim to minimise discomfort, but some patients experience temporary post-treatment sensitivity or discomfort. It fades away, but it's something to keep in mind.
- Adjacent Tooth Health: A root canal-treated tooth affects the health of neighbouring teeth. The tension of biting and chewing causes long-term problems in neighbouring teeth.
- Recurrent Infections: The treated tooth develops a new infection in rare instances, requiring retreatment or extraction. It occurs if bacteria find their way back into the root canal system.
- Limited Longevity: Many root canal-treated teeth last a lifetime, but some require retreatment or develop issues over time. Regular dental check-ups are important to monitor the health of root canal-treated teeth.
- Complex Anatomy: The intricate anatomy of root canals makes complete cleaning and sealing challenging, especially in teeth with unusual or curved root canals.
- Overall Tooth Condition: Root canal treatments aren’t suitable for teeth with poor oral health or those surrounded by gum disease, as these factors impact the success of the procedure.
How Much Does the Root Canal Treatment Cost?
The cost of a root canal treatment varies based on factors such as the location of the dental clinic, the tooth's location in the mouth, the complexity of the case, and whether additional procedures or restorations are needed. The cost of a root canal procedure in Turkey is £60 per canal with an included X-ray. The actual cost differs between clinics and centres.
The condition of the particular tooth affects the cost of a root canal procedure. Teeth with more canals or complicated root structures require more time and expertise, which impacts the cost. The need for a dental crown after the root canal contributes to the total expense.
The ability of a root canal treatment to save a tooth from extraction, avoid additional complications, and relieve pain frequently justifies its cost. Dental insurance plans provide coverage for a portion of the cost, depending on the terms of the policy.
A dental provider must be consulted to obtain an accurate estimate for a root canal procedure. They evaluate the patient's individual case, assess the tooth's condition, and provide a detailed breakdown of the expected costs. Prioritising one’s dental health and considering the long-term benefits of preserving natural teeth is important when evaluating the cost of a root canal treatment.
How Long Does the Root Canal Treatment Take?
Root canal procedures take anywhere from a few hours to a few days, depending on the severity of the infection, the complexity of the affected tooth, and other factors. The average time for a single root canal procedure is between 60 and 90 minutes. The entire root canal treatment process involves a few appointments over the course of a few weeks.
The total number of visits needed for a root canal treatment varies. One visit is sufficient to complete the entire treatment. Multiple canals, grave infections, or the need for additional treatments necessitate more than one visit and extend the process over several days.
Patients experience mild discomfort or sensitivity for a few days following the procedure in terms of root canal recovery time. The discomfort is manageable with over-the-counter pain relievers and must gradually subside. Most individuals are able to resume their regular activities the day after the root canal treatment, but it's advisable to avoid chewing on the treated tooth until the crown is placed.
Consult a dentist for specific information about the expected number of visits and the duration of the root canal treatment. Providing personalised guidance according to the patient's dental condition and individual needs.
Does Dental Crown Requires Root Canal Treatments?
No, not all dental crowns call for root canal treatment. A dental crown is meant to mend and secure a damaged or weakened tooth. Root canal procedures are sometimes necessary in order to save a tooth.
A tooth that has suffered severe decay, damage, or infection that has penetrated the inner pulp necessitates root canal treatment prior to having a crown placed. The infected or damaged pulp is extracted during the root canal procedure, and the canals are rinsed after, decontaminated, capped, and sealed. Ensuring that the tooth is free from infection and provides a stable foundation for the crown.
A dental crown is placed without root canal treatment if the pulp is healthy. The crown serves to reinforce and protect the tooth as it restores its appearance and functionality. Root canals are needed if decay or trauma damages the pulp.
The decision to perform a root canal treatment alongside a dental crown placement depends on the patient's tooth's condition. A thorough evaluation by a dentist determines whether a root canal is needed to guarantee the efficacy and longevity of the dental crown and the total health of the tooth.
Does Dental Onlays Require Root Canal Treatments?
No, dental onlays don’t require root canal treatment. The tooth beneath the onlays needs root canal treatment approximately 5% of the time. Dental crowns cover the entire tooth, whereas onlays just restore a portion of it. They’re used when the damage or decay is extensive but doesn’t affect the inner pulp of the tooth.
A root canal procedure isn’t necessary before placing a dental onlay in cases where the tooth's pulp remains healthy and unaffected by the damage. Onlays are crafted to fit precisely into the damaged area of the tooth, restoring its structure and functionality while preserving the natural tooth material.
A root canal is required before an onlay is placed if the damage or decay has progressed to the point where it has reached the tooth's pulp and caused infection or inflammation. The root canal procedure addresses the inner pulp issues, removing the infection, cleaning and disinfecting the tooth's interior, and sealing the root canals. Once the tooth is infection-free, an onlay is placed to restore its appearance and function.
The need for a root canal in conjunction with dental onlays depends on the condition of the tooth. A dental professional determines if a root canal is required before placing an onlay by assessing the damage and pulp health.
Can the Root Canal Treatment Prevent Cavities?
No, a root canal treatment cannot prevent cavities. A cavity is a crack in the tooth that results from decay. A person with a cavity is advised to consult a dentist to get a filling. A root canal treatment is needed if the cavity in the tooth continues to spread and deepen. The procedure is done to save a tooth that has already been damaged or made weak by an infection or other problem that has reached the inner pulp of the tooth. Eliminating the infection prevents further damage to the tooth, but it doesn’t prevent the formation of cavities on other teeth or on the treated tooth's surface.
Bacterial activity on the tooth's surface is what primarily causes tooth cavities. Sugary diets, poor oral hygiene, and inadequate dental care lead to the development of cavities over time. The decay process begins on the outer enamel layer of the tooth and progresses inward.
Maintaining good oral hygiene practises, including regular brushing, flossing, and professional dental cleanings, is crucial to preventing cavities. Reducing sugar intake, using fluoride toothpaste, and following a well-balanced diet help minimise the risk of developing new cavities. Cavity prevention requires ongoing oral care and preventive measures, while a root canal treats existing issues within a tooth.





