Gingivitis is a common and mild form of gum disease that affects the gums, causing inflammation, redness, and bleeding. Gingivitis is the earliest stage of periodontal disease and, if left untreated, progresses to more severe conditions, such as periodontitis. Understanding what causes gum disease is essential for effective prevention and treatment. Plaque buildup, poor oral hygiene, smoking, hormonal changes, certain systemic diseases, medications, and poor nutrition are among the primary contributors to gum infection and gingivitis.
Gingivitis treatment focuses on reducing inflammation and removing dental plaque deposits. Essential gum disease treatments include improved oral hygiene practices like regular tooth brushing, flossing, and professional dental cleanings. Plaque and tartar must be removed from above and below the gum line with scaling and root planing for more severe cases. Medications, including antiseptic mouthwashes and antibiotics, are used with mechanical treatments to control bacterial infections. Addressing underlying causes, such as nutritional deficiencies or changing medicines that induce gum overgrowth, enhances treatment outcomes.
Saltwater rinses and other alternative treatments help ease symptoms using their antiseptic and anti-inflammatory properties. These alternative treatments must not replace professional care. Maintaining good oral hygiene and seeking regular dental check-ups prevents and effectively manages gingivitis and ensures long-term gum health.

What is Gingivitis?
Gingivitis is a type of dental problem characterised by inflamed gum tissue. Gingivitis is the earliest stage of gum disease and develops as plaque, tartar, and bacteria accumulate on the teeth, leading to gum infection. Gum disease is another term used interchangeably with gingivitis.
Gingivitis represents the initial phase of gum disease, a more extensive dental issue. The primary cause of gingivitis is the buildup of plaque, a sticky film of bacteria on the teeth. Plaque turns into tartar if not appropriately removed through good oral hygiene. It makes it easier for bacteria to grow and causes more inflammation. The common symptoms of gingivitis include red, swollen, and bleeding gums during brushing or flossing.
Effective management of gingivitis involves routine dental cleanings by a professional and good oral hygiene at home, including brushing twice daily and flossing daily. Periodontitis is a severe form of gum disease that leads to tooth loss if it isn't treated. Untreated gingivitis, a mild gum problem, progresses to more severe complications.

How common is Gingivitis?
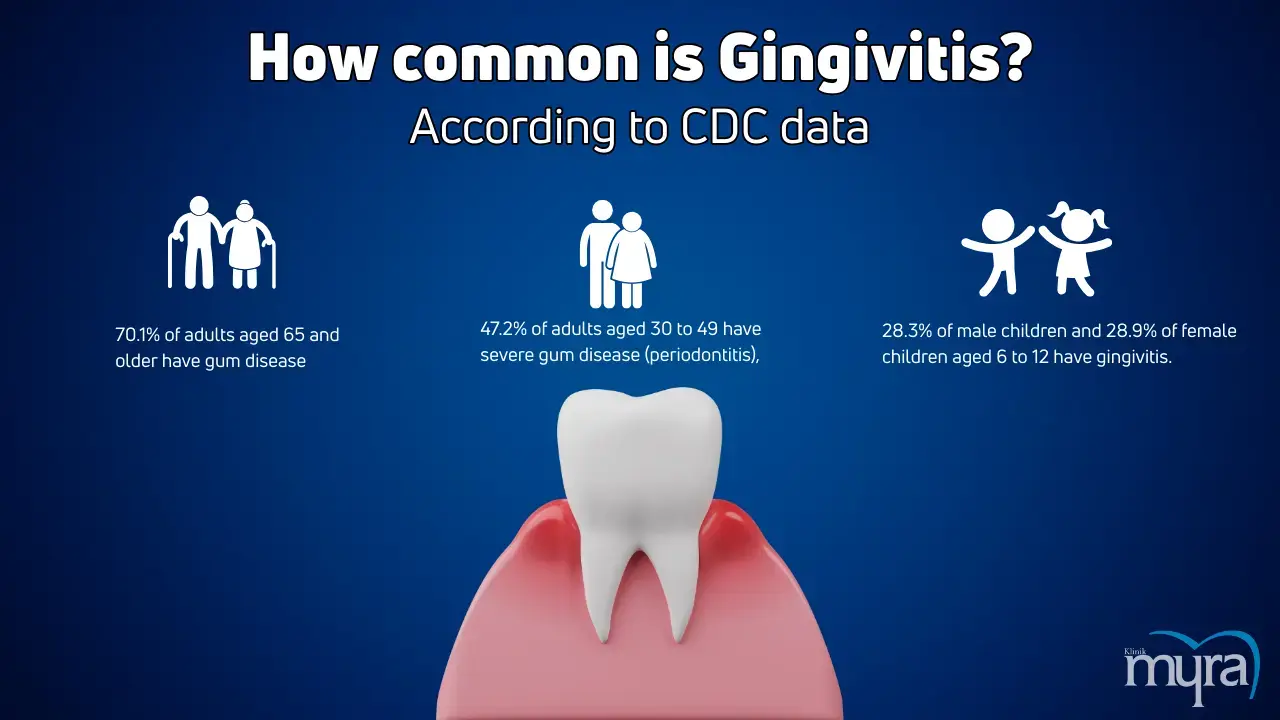
Gingivitis is a common dental problem among adults in the United States. Gingivitis is reversible with proper oral hygiene practices. The U.S. Centers for Disease Control and Prevention (CDC) says that 70.1% of adults aged 65 and up have gum disease, and 47.2% of adults aged 30 to 49 have severe gum disease (periodontitis). A study on children aged 6-12 found similar prevalence rates of gingivitis in males (28.3%) and females (28.9%).
A study found that gingivitis was higher in males, with 55.1% affected compared to 42.7% of females. Another study indicated no significant difference between males (28.3%) and females (28.9%). The prevalence of gingivitis in females is reported variably, with some studies showing a lower prevalence compared to males (42.7% vs. 55.1%).
The prevalence of gingivitis highlights the widespread nature of a tooth problem. Variations in reported rates between studies underscore the need for more comprehensive research to understand epidemiologic trends across various populations and age groups. Gingivitis remains a significant concern as it progresses to more severe forms of gum disease if left untreated. Emphasizing good oral hygiene practices and regular dental check-ups is crucial for preventing and managing gingivitis.
What are the types of Gingivitis?
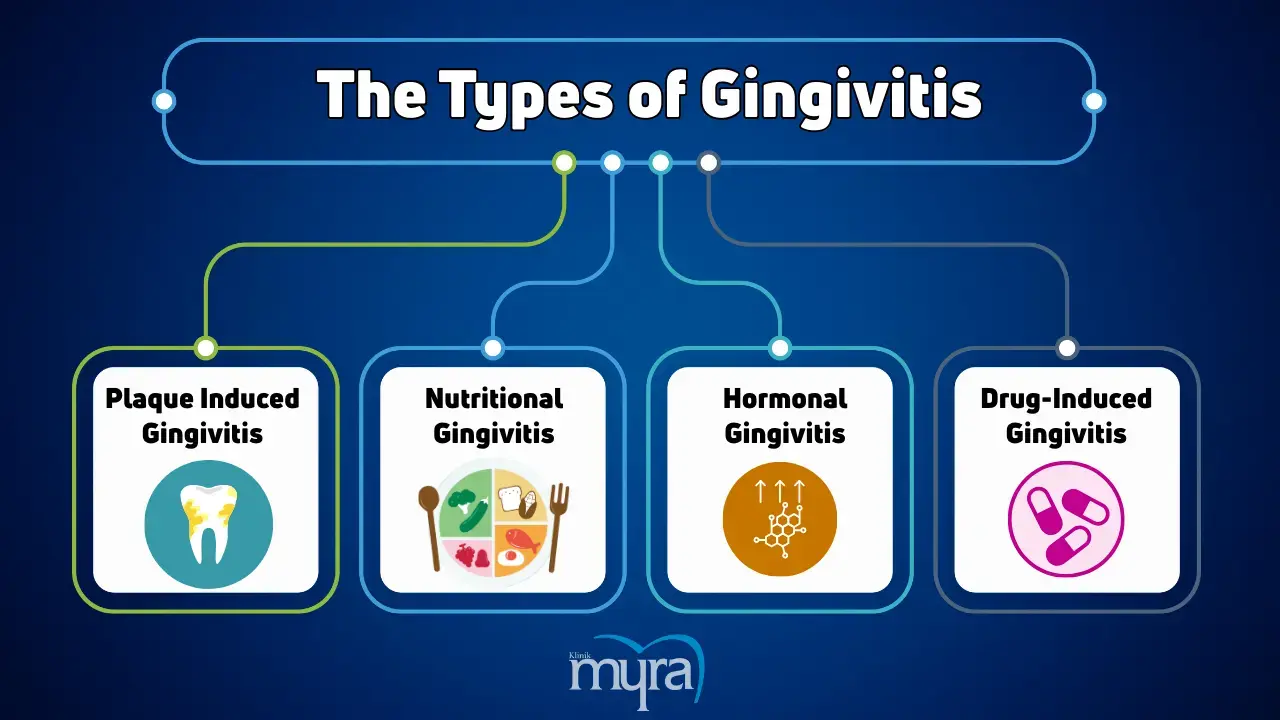
The types of Gingivitis are listed below.
- Plaque Induced Gingivitis: The most prevalent type of gingivitis, plaque-induced gingivitis results from plaque buildup, a sticky bacterial film that develops on teeth. Poor oral hygiene leads to plaque buildup, which irritates the gums, causing inflammation, redness, and bleeding.
- Nutritional Gingivitis: A type of gingivitis that occurs due to deficiencies in essential nutrients, such as vitamin C. Lack of proper nutrition weakens the gums and makes them more susceptible to infections and inflammation.
- Hormonal Gingivitis: Hormonal changes during puberty, pregnancy, menstruation, or menopause lead to an increased risk of gingivitis. The changes make the gums more sensitive and prone to inflammation, even with a small amount of plaque.
- Drug-Induced Gingivitis: Certain medications cause gingival overgrowth or inflammation as a side effect. Drugs such as anticonvulsants, immunosuppressants, and calcium channel blockers help with gingivitis by affecting gum tissue health and the reaction to plaque.
1. Plaque Induced Gingivitis
Plaque-induced gingivitis results from the buildup of plaque on the teeth. Plaque is a sticky film of bacteria, food residue, saliva, and mucus combined with calcium and phosphate salts. Poor oral hygiene allows plaque to build up between the teeth and gums, leading to inflammation and infection of the gums.
Plaque-induced gingivitis affects the crevice (sulcus) between the tooth and the gingiva (gums). The irritation from plaque deepens the crevice, forming gingival pockets that harbour bacteria responsible for gingivitis and root caries.
Plaque-induced gingivitis results from dental plaque buildup rather than hormonal changes, systemic disorders, medications, nutritional deficiencies, or heavy metal exposure. Hormonal changes, systemic disorders, and certain medications exacerbate plaque-induced gingivitis but are not primary causes. It is the most common form of gingivitis, unlike non-plaque-induced gingivitis, which occurs less frequently and results from infections, allergic reactions, trauma, mucocutaneous disorders, or hereditary conditions. Symptoms like red, swollen, and bleeding gums are common across all types. Things in the area like bad teeth grinding, dental calculus, food getting stuck in the teeth, broken dental restorations, and dry mouth worsen plaque-induced gingivitis without being the leading causes.
2. Nutritional Gingivitis
Nutritional gingivitis is a gum disease resulting from deficiencies in essential nutrients, particularly vitamin C. Modern eating habits, including eating more refined carbohydrates and having an unhealthy balance of omega-6 to omega-3 fatty acids, worsen gum inflammation. Dietary factors contribute to inflammation through mechanisms involving the activation of NFkB and oxidative stress.
Nutritional gingivitis primarily affects the gums, causing inflammation, swelling, and bleeding. The deficiency in essential nutrients weakens the gum tissue, making it more susceptible to infections and inflammation. Gingivitis, which affects the space between the teeth and gums, differs from nutritional deficits that weaken the gum tissue.
The difference between nutritional gingivitis and plaque-induced gingivitis is that the latter is caused by an imbalance of vital nutrients, particularly vitamin C, while an excess of dental plaque causes plaque-induced gingivitis. Changes in hormones cause hormonal gingivitis, and some medications cause drug-induced gingivitis. The patient's diet has a lot to do with nutritional gingivitis. The inflammatory process in nutritional gingivitis is promoted by high glycemic index carbohydrates, which activate NFkB and oxidative stress. It differs from the bacterial cause of plaque-induced gingivitis and the hormonal or medicinal influences of hormonal and drug-induced gingivitis. Nutritional gingivitis underscores the importance of a balanced diet in maintaining gum health, unlike other types that are more influenced by oral hygiene, hormonal fluctuations, or side effects.
3. Hormonal Gingivitis
Hormonal gingivitis is a gum disease caused by rapid changes in hormone levels. The shifts affect the gums, leading to an exaggerated inflammatory reaction and even minor plaque accumulation. Symptoms worsen during menstruation, menopause, pregnancy, and puberty.
Hormonal gingivitis affects the gingival tissues, which are the gums surrounding the teeth. The hormonal fluctuations increase blood flow and sensitivity in the gums, causing inflammation, swelling, and bleeding, particularly around the gum line where plaque accumulates. The gums become more susceptible to irritation and inflammation even with minimal plaque presence.
The primary cause of hormonal gingivitis is a change in hormone levels, such as during puberty, pregnancy, menstruation, and menopause. A lack of vital nutrients causes nutritional gingivitis, while the inflammatory response in hormonal gingivitis is heightened due to increased blood vessel dilation and the influence of oestrogen levels. Gum inflammation worsens, while plaque development is relatively minor.
4. Drug-Induced Gingivitis
Drug-induced gingivitis develops when a patient takes medication for a systemic condition. The medicines include anticoagulants, fibrinolytic agents, oral contraceptives, protease inhibitors, phenytoin (for seizures), calcium channel blockers (for angina and high blood pressure), and vitamin A and its analogues. The metabolites of these drugs induce the proliferation of fibroblasts, leading to gingival inflammation.
Drug-induced gingivitis affects the gingival tissues, or gums, surrounding the teeth. The medications cause an imbalance between the synthesis and degradation of the extracellular matrix, accumulating immature proteins and collagen in the extracellular matrix. The buildup leads to inflammation, swelling, and overgrowth of the gum tissue.
Drug-induced gingivitis differs from other types of gingivitis in its cause and mechanism. Plaque-induced gingivitis is caused by dental plaque buildup, insufficient nutrients cause nutritional gingivitis, and the side effects of some medications cause drug-induced gingivitis. The inflammatory response in drug-induced gingivitis is driven by drug metabolites that induce fibroblast proliferation and collagen accumulation, unlike hormonal gingivitis, which is caused by hormonal fluctuations. Drug-induced gingivitis is linked to the use of medications, whereas other types of gingivitis are associated with poor oral hygiene, dietary factors, or hormonal changes.
What Causes Gingivitis?
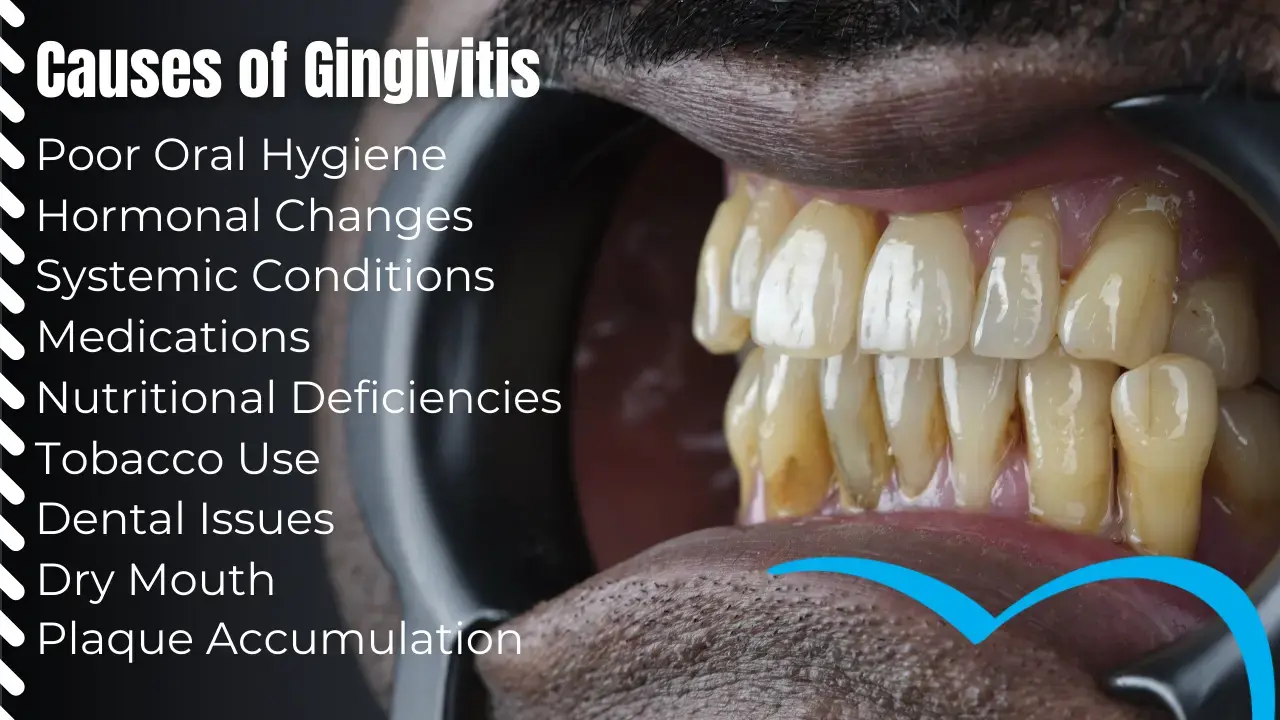
The causes of gingivitis are listed below.
- Poor Oral Hygiene: Inadequate oral care practices, such as not brushing and flossing regularly, allow plaque to build up on the teeth. The buildup leads to irritation and swelling of the gums, a hallmark of gingivitis.
- Hormonal Changes: Hormonal fluctuations during puberty, pregnancy, menstrual cycles, and menopause make gums more sensitive and prone to inflammation. The changes exacerbate the inflammatory response to plaque, leading to gingivitis.
- Systemic Conditions: Certain health conditions, such as diabetes, HIV/AIDS, leukaemia, and other conditions that affect the immune system, increase the risk of gingivitis. The conditions reduce the body's ability to fight infections, including germs affecting the gums.
- Medications: Some medications, including phenytoin (used for epileptic seizures), calcium channel blockers (used for angina and high blood pressure), anticoagulants, fibrinolytic agents, oral contraceptives, and protease inhibitors, cause gingivitis as a side effect. The drugs lead to gum overgrowth and inflammation.
- Nutritional Deficiencies: A lack of essential nutrients such as vitamin C leads to gingivitis. Poor nutrition weakens the immune system and affects the health of the gums, making them more susceptible to inflammation and infection.
- Tobacco Use: Smoking or chewing tobacco is a risk factor for gingivitis. Tobacco use impairs blood flow to the gums, reduces the immune response, and promotes plaque accumulation, contributing to gum disease.
- Dry Mouth: Conditions that cause dry mouth (xerostomia) increase the risk of gingivitis. Saliva helps cleanse the teeth and gums, so a lack of saliva increases plaque formation and gum irritation.
- Dental Issues: Poorly fitting dental appliances, such as bridges, fillings, dental implants, or crooked teeth that are difficult to clean, contribute to gingivitis. The issues create areas where plaque accumulates and irritates the gums.
- Plaque Accumulation: The primary cause of gingivitis is plaque accumulation on the teeth. Plaque is a sticky, colourless film of bacteria, food particles, saliva, and mucus. Plaque hardens into tartar if the patient does not brush and floss their teeth regularly, which makes the gums hurt even more.
What are the Symptoms of Gingivitis?
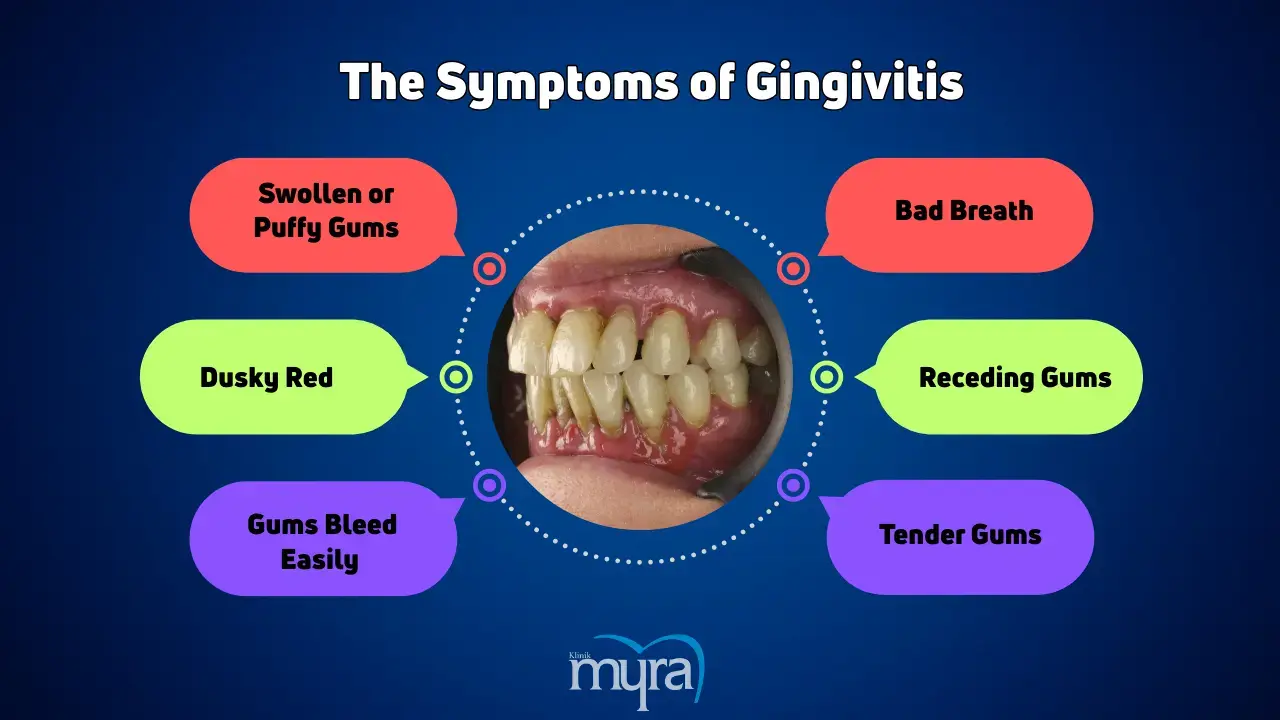
The symptoms of Gingivitis are listed below.
- One of the signs of gingivitis is swelling or puffiness of the gums, which makes them look bigger than normal.
- A sign of gum disease is gums that are dusky red or darker in colour than their usual pink hue.
- Gingivitis symptoms include gums that bleed easily during brushing or flossing, indicating inflammation and irritation.
- Persistent bad breath, or halitosis, is a common sign of gum disease. The bacteria present in plaque and tartar buildup frequently cause it.
- One of the advanced gingivitis symptoms is receding gums, which occur when the gums pull back from the teeth, exposing more of the tooth's outer layer or root.
- Tenderness or pain in the gums is a sign of inflammation and one of the signs of gum disease, making the gums sensitive to touch or pressure.
1. Swollen or puffy gums
Swollen or puffy gums result from the enlargement and puffiness of the gum tissue, which is a sign of underlying dental issues. The condition is characterised by the gums appearing larger than usual, feeling tender to the touch, and sometimes bleeding during brushing or flossing.
Inflamed gums surrounding the teeth are a sign of gingivitis. Gingivitis occurs when plaque, a sticky film containing bacteria, accumulates along the gumline. The plaque buildup leads to gum inflammation as the immune response fights off the bacteria. The inflammation causes “swollen gums around tooth,” which are tender and irritated. Regular brushing and flossing are necessary to remove plaque, but failing to do so results in the formation of tartar, which exacerbates gingivitis symptoms and irritated gums. Bacteria in plaque and tartar trigger an immune response, leading to gum inflammation and swelling. The loss of gum tissue and bone around teeth results from periodontitis, a more severe form of gum disease if the condition is not treated.
Maintaining excellent oral hygiene practices, such as regular brushing, flossing, and dental check-ups, is crucial for preventing and managing puffy gums caused by gingivitis. Failure to reduce swelling despite these efforts requires a visit to a dentist for a complete checkup and the right treatment to avoid more problems.
2. Dusky red
Dusky red gums refer to a darkened, deep red colouration of the gum tissue, indicating an advanced stage of inflammation and irritation. The colour change indicates gum disease and is associated with gingivitis.
Dusky red gums are a clear sign of gum inflammation, a hallmark of gingivitis. Gingivitis is an infection caused by bacteria that builds up on the teeth due to plaque. Plaque irritates the gums when it builds up and is improperly removed by brushing and flossing. The irritation, in turn, causes the gums to become inflamed and swollen. The inflammation increases blood flow to the affected areas, resulting in the gums' darker, dusky red appearance. Swollen gums around the tooth and irritated gums exacerbate the condition, making the redness more pronounced. The dusky red indicates a stronger response to ongoing infection and inflammation than the bright red, which is common in early gingivitis. Serious gum disease, including periodontitis, develops from the condition if not treated, causing substantial loss of tissue and bone surrounding the teeth. Recognising and addressing dusky red gums early through proper oral hygiene and professional dental care is crucial to preventing further complications.
3. Gums that bleed easily when you brush or floss
Gums that bleed easily when you brush or floss refer to the tendency of the gum tissue to bleed with minimal provocation, such as during routine oral hygiene practices. The bleeding is a symptom of underlying gum inflammation and irritation.
A common sign of gingivitis is bleeding gums while brushing or flossing. Tartar, plaque, and bacteria build up along the gumline. Gum inflammation happens because the buildup irritates the gums. An irritated and inflamed gum loses its healthy pink colour and begins to pull away from the teeth, which causes “swollen gums around tooth.” The inflammation makes the gums more sensitive and prone to bleeding. The irritated gums easily bleed when brushed or flossed because of pressure. The gum tissue is so weak and infected that it bleeds because of the body's immune system's reaction to the bacterial infection in the plaque. Regular and proper oral hygiene manages and reduces these symptoms. A dentist needs to look at gums that keep bleeding so they do not worsen and become more serious oral diseases.
4. Bad breath
Bad breath, or halitosis, is an unpleasant odour emanating from the mouth. Bad breath is persistent and noticeable to others, especially in cases of severe gum disease.
Gingivitis causes bad breath because oral bacteria produce sulphur compounds and other unpleasant odorants. The bacteria thrive on plaque accumulating along the gumline, leading to gum inflammation and irritation. The inflamed gums swell with the progression of gingivitis, making spaces around the teeth for additional bacteria to hide. Bacterial action results in compounds with an odour similar to sulphur or rotten eggs, exacerbating bad breath.
The presence of irritated gums and “swollen gums around tooth” exacerbates the condition, making the unpleasant odour more pronounced. The inflammation and bleeding associated with gingivitis further promote bacterial growth, intensifying the bad breath. Maintaining good oral hygiene practices, such as regular brushing, flossing, and dental check-ups, helps manage gingivitis and reduce bad breath. Seek the advice of a dentist to get a proper diagnosis and treatment for periodontal disease if these symptoms continue.
5. Receding gums
Receding gums occur when the gum line around a tooth thins or pulls back, revealing more of the tooth's root or enamel. The exposed tooth structure creates spaces between the gums and teeth, which are ideal breeding grounds for bacteria that cause cavities.
Receding gums are a symptom of the early stage of gum disease. Plaque buildup along the gumline causes gum inflammation, a defining feature of gingivitis. The accumulation of plaque, a sticky film of bacteria, irritates the gum tissue, leading to “swollen gums around tooth” and irritated gums. The irritation and inflammation cause the gums to pull back from the teeth. Regression of inflamed gum tissue occurs due to the body's immune response attempting to combat the bacterial irritants found in plaque.
The recession exposes more of the tooth surface and creates pockets where bacteria accumulate, exacerbating the problem. Receding gums in gingivitis indicate that the gum tissue is adversely affected by bacterial plaque and gum inflammation. Insists on the importance of finding gum disease early and taking action to stop it from getting worse.
6. Tender gums
Tender gums, or sore gums, are a condition where the gums feel sensitive, painful, or sore to the touch. The sensitivity is an indication of underlying inflamed and irritated gums.
Tender gums are a common symptom of gingivitis, the early and mildest form of gum disease. Gingivitis occurs due to plaque accumulation along the gumline, leading to inflammation and irritation of the gum tissue. Plaque, a sticky film of bacteria, builds up on the teeth and gums, causing an immune response from the body. The response results in gum inflammation, leading to irritated and “swollen gums around tooth.” The inflammation makes the gums more sensitive and tender, causing discomfort or pain when touched or while eating and brushing.
The tenderness is the body's way of signalling an issue with oral health, specifically the presence of bacterial plaque causing gum inflammation. Gingivitis, if untreated, worsens periodontitis and other gum diseases, which permanently harm the gums and teeth. Pay attention to gums that hurt and maintain good oral hygiene habits like brushing, flossing, and regular dental checkups to stop and treat gingivitis before it worsens.
Does gingivitis have long term side effects?
Yes, gingivitis does have long-term side effects if left untreated. Periodontitis is a more advanced stage of gum disease that develops from gingivitis if left untreated. The health of the gums and bones supporting the teeth declines as tartar and plaque accumulate. Periodontal pockets form as the gum tissue begins to pull away from the teeth, allowing harmful bacteria to go beyond where brushing and flossing reach. The long-term risks of untreated periodontal disease include gum recession, bone damage, and tooth loss. Advanced periodontal disease exacerbates other inflammation-related illnesses and has been linked to severe health issues such as heart disease, diabetes, arthritis, and stroke. Regular dental exams and appropriate periodontal disease treatment are essential to prevent these severe consequences.
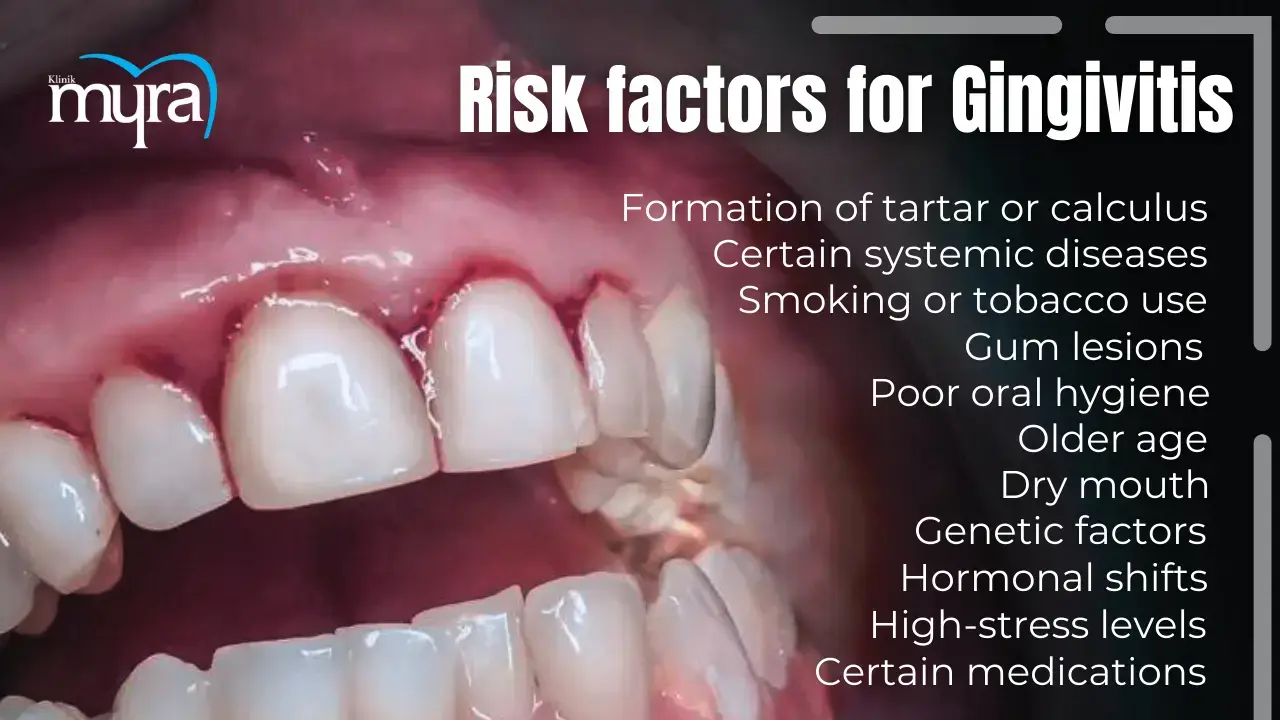
What are the risk factors for Gingivitis?
The risk factors for Gingivitis are listed below.
- Older age: Higher rates of periodontal disease are associated with ageing, with over 70% of Americans over age 70 having some level of periodontal disease.
- Genetic factors: Genetics makes some people more susceptible to developing gum disease.
- Gum lesions: Lesions are worsened by plaque, even if not directly caused by dental bacterial plaque.
- Poor oral hygiene: Inconsistent or irregular brushing and flossing, or consistently missing the same areas of the mouth, allow plaque to accumulate and lead to gingivitis.
- Formation of tartar or calculus: A hardened plaque that cannot be removed by brushing alone irritates the gums and contributes to gingivitis.
- Dry mouth: A consistent lack of saliva leads to increased plaque buildup, increasing the risk of gingivitis.
- Smoking or tobacco use: Smoking or using tobacco has a profound negative effect on gingival tissues, doubling the risk of gum disease compared to non-smokers.
- Certain systemic diseases and conditions: Diseases such as diabetes, leukaemia, cancer, and HIV, hinder the body's ability to fight off infections, including gum disease.
- Hormonal shifts: Changes during puberty, menstruation, pregnancy, menopause, or from oral contraceptives cause increased sensitivity in the gums.
- High-stress levels: High-stress levels weaken the immune system and impair the body's ability to fight infections like gum disease.
- Poor nutrition and an unbalanced diet: Lack of vital nutrients makes it more difficult for the body to prevent infections like gum disease.
- Certain medications and drugs: Medications such as steroids and oral contraceptives make individuals more susceptible to gum disease.
What are the Complications of Gingivitis Infection?
The complications of Gingivitis Infection are listed below.
- Bleeding gums: One of the initial complications of gum disease is bleeding gums. Healthy gums must look pink and not bleed. Gingivitis begins to manifest when the gums bleed while brushing or flossing.
- Receding gums: Gum disease is a primary cause of receding gums, where the gum tissue surrounding a tooth begins to pull back or wear away, exposing the tooth root and making teeth appear longer.
- Bad breath: Bad breath is a common symptom of gingivitis. Bacteria associated with gum disease produce foul odours while breaking down food particles in the mouth. Some bacteria cause bad breath that does not go away even after brushing or rinsing.
- Tooth loss: Untreated gum disease progresses to periodontitis, which attacks the entire tooth support system, including soft tissue and bone. The damage results in teeth becoming loose and eventually leads to tooth loss.
Is Gingivitis a Serious Condition?
Yes, gingivitis is a serious condition. Patients with gingivitis have mild symptoms, but they must not be ignored. Periodontitis is a more severe problem if it is not treated. The cause of gingivitis is poor oral hygiene, which allows plaque to build up on the teeth and irritate the surrounding gum tissue. The plaque hardens into tartar, further aggravating the gums and creating a protective environment for harmful bacteria.
Untreated gingivitis separates the gums from the teeth, causing tissue and bone damage that supports the teeth. The damage makes the teeth loose and unstable, leading to tooth loss if the infection progresses. Gingivitis has been linked to other systemic health issues such as respiratory disease, diabetes, coronary artery disease, stroke, and rheumatoid arthritis. The bacteria responsible for periodontitis enter the bloodstream through the gum tissue, affecting other body parts.
Take gingivitis seriously and seek prompt treatment from a dental professional if symptoms, such as red, swollen, or bleeding gums, are present. Early detection and treatment prevent gingivitis from becoming periodontitis.
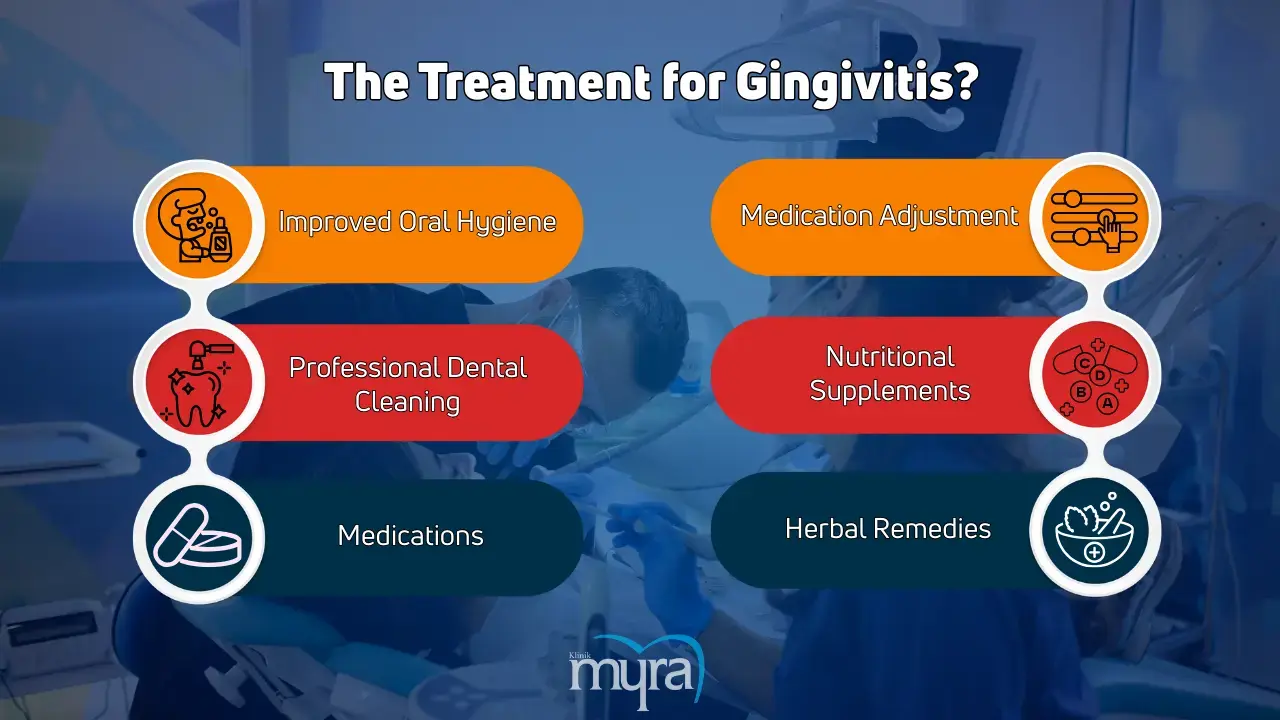
What are the treatment for Gingivitis?
The treatments for Gingivitis are listed below.
- Improved Oral Hygiene: Regular tooth brushing with an appropriate technique and interproximal hygiene practices such as flossing or using interproximal brushes are essential. The methods help manage and prevent the progression of gingivitis by effectively removing plaque buildup, which is crucial in the initial stages of the condition.
- Professional Dental Cleaning: Scaling and root planing performed by a dental professional are necessary to remove plaque and tartar (calculus). The procedures are vital for severe gingivitis treatment as they eliminate hardened deposits that are unremovable by regular brushing, ensuring thorough cleaning of the gum line.
- Medications: Antiseptic mouthwashes containing chlorhexidine are prescribed with mechanical plaque removal. The medications help reduce dental biofilm and control inflammation and infection in the gums, making them a significant component of “how to treat gingivitis.”
- Medication Adjustment: Changing the medicine improves the treatment outcome in cases of drug-induced gingival overgrowth. The adjustment helps reduce gingival inflammation and overgrowth by addressing the root cause related to medication side effects.
- Nutritional Supplements: Prescribing supplements in cases of gingivitis due to nutritional deficiencies supports overall gum health. Ensuring the intake of essential nutrients helps resolve gingivitis caused by a lack of vital vitamins and minerals, contributing to the healing process.
- Herbal Remedies: Medicinal or herbal plants such as pomegranate, tea, and chamomile, known for their anti-inflammatory properties, are used. These plants help reduce gingival bleeding and inflammation and are prescribed conventional treatments like scaling for a synergistic effect.
How much does it Cost for treatment of Gingivitis?
The cost of treating gingivitis ranges from £49 to £2500 but varies depending on the severity of the condition and the type of treatment required. A basic dental cleaning, called prophylaxis, is one of the most common and cost-effective treatments for gingivitis, costing around £49. The procedure involves removing plaque and tartar from the teeth and gums. Periodontal scaling, a slightly more intensive procedure, averages around £99 and focuses on cleaning above and below the gum line to remove plaque and tartar.
A more comprehensive treatment approach is necessary for more advanced cases of gingivitis, which increases the cost. Periodontal scaling and root planing, a deep cleaning procedure that removes plaque and tartar below the gum line, range from £165 to £405. Surgical intervention is required in the most severe cases, driving the cost up to £2500.
The cost of gingivitis treatment includes the materials used, the specific body parts involved, and the required procedures. The type and extent of the dental materials, such as antiseptic mouthwashes, medicated gels, or specialised cleaning instruments, influence the cost. The condition of the gum tissue and underlying bone structure plays a role, as more advanced deterioration requires more complex and costly procedures. The specific procedures, from basic cleanings to more invasive surgical interventions, impact the total expense. Dental insurance coverage alleviates some of these costs, with most plans covering a portion of basic cleanings and some types of gum disease treatment.

Can Turkey Teeth Procedure cause Gingivitis?
No, the non-invasive Turkey Teeth procedure does not cause gingivitis. Gingivitis is typically caused by factors like poor oral hygiene or complications following dental procedures. The non-invasive nature of the Turkey Teeth procedure, such as crown placement or veneer application, does not involve excessive tooth filing or significant alterations to the natural tooth structure, which are common risk factors for gum inflammation.
However, complications after the Turkey Teeth procedure, such as sensitivity, crowns or veneers falling out, or gum infections, can create conditions that increase the risk of gingivitis. These complications can make the gums more vulnerable to bacterial infections, leading to inflammation.
It's important to choose a reputable and experienced dental professional for Turkey Teeth procedures to minimize complications and maintain good oral health. By following proper post-procedure care, the risk of gingivitis can be significantly reduced.
Can antibiotics treat Gingivitis?
Yes, antibiotics can treat gingivitis, but they are not recommended as the sole treatment. Antibiotics are used as a medicine for gingivitis to help control bacterial infections associated with the condition. Antibiotics do not eliminate all the bacteria responsible for gingivitis, which means some bacteria remain and reactivate the infection.
Gingivitis is effectively managed and controlled through full mouth disinfection, which includes thorough professional cleaning and improved oral hygiene practices. Relying solely on antibiotics is not advisable due to the risk of bacterial resistance, which occurs when bacteria become more assertive and less responsive to antibiotic treatment. The resistance complicates the future treatment of infectious diseases.
Antibiotics must be reserved for situations where full mouth disinfection alone does not control the infection. Combining antibiotics with other treatments, such as professional dental cleaning and proper oral hygiene, provides a more comprehensive method for dealing with gingivitis and reducing the risk of coming back.
Does using saltwater for Gingivitis help?
Yes, using salt water for gingivitis helps. Saltwater is a beneficial alternative treatment for gingivitis due to its anti-inflammatory and antiseptic properties. Saltwater helps reduce gum inflammation, eliminate microorganisms in the mouth, and promote healing of the gums. A saltwater mouthwash helps ease the pain of gingivitis and speed up the gums' natural healing process.
Making saltwater mouthwash is as simple as mixing one teaspoon of salt with one cup of warm water. Stir the mixture until the salt is completely dissolved, then gargle with the solution for 30 seconds to 1 minute. It is done multiple times daily or as a dentist directs.
Saltwater does a good job of relieving the symptoms of gingivitis, but it must not be used instead of good oral hygiene or regular dental checkups. Maintaining healthy gums requires consistent brushing and flossing, professional cleanings and evaluations by a dentist. Saltwater is an alternative medicine for gingivitis, but comprehensive oral care is needed to prevent recurrence and ensure oral health.
How long does it take to Recover from Gingivitis?
It takes 10 to 14 days to recover from gingivitis. The duration of recovery varies based on the severity of the ailment and the timeliness and efficacy of therapy.
Gingivitis is managed with diligent oral hygiene practices, including frequent brushing and flossing and routine visits to the dentist or dental hygienist for professional cleaning. Scaling and root planing are professional procedures that effectively eliminate plaque and tartar from the surface and the area behind the gum line, providing comprehensive therapy for the problem.
Many individuals observe improvements in gum health within a few weeks of initiating treatment, but the specific timeframe may vary across individuals. Severe instances of gingivitis necessitate an extended recuperation period spanning several months. Proper dental hygiene guarantees complete recuperation and guards against future relapses. The recommended oral hygiene routine consists of brushing teeth twice daily, flossing at least once per day, and regularly using an antimicrobial mouthwash. Regular dental check-ups are crucial for monitoring gum health and swiftly addressing any initial indications of gum disease.






