An autograft is a surgical procedure involving the removal of tissue or cells from one area of an individual's body and then transplanting them to another area of the same body. An autograft differs from an allograft, which involves the transplantation of tissue from one individual to another.
Transplantation is made difficult by the immune system’s tendency to attack foreign objects, such as organs, that are detected as threats. Autografts avoid the problem due to the transplanted tissue or cells being from the same body.
Autografts have increased success rates because the body recognises the transplanted tissues as its own, preventing immune reactions from being mounted against them. Autograft procedures aim to treat illnesses that cause significant tissue loss or damage. For instance, an autograft enables the replacement of a lost bone with healthy bone tissue from another area of the same body in cases where the bone was lost as a result of an injury or disease.
An autograft stem cell transplant procedure is a type of autografting method. The patient's stem cells are removed in the procedures. Stem cells have the capacity to differentiate into different types of cells.
Stem cells are reintroduced into the patient's body following therapy, such as high-dose chemotherapy or radiation therapy, to aid in the restoration of function within the immune system. The Melphalan autograft is one example of a stem cell autograft. Melphalan is a chemotherapy drug that is used to kill cancer cells in cancer treatments.
Patients undergoing chemotherapy using drugs like Melphalan, receive autografted stem cells to aid in the recovery and replacement of the blood cells lost to chemotherapy. The answer to the query “What is autograft?” is a procedure where healthy tissue or cells are removed from one part of the body and transferred to the area that requires them. The method of transplantation and the harvesting procedure differ depending on the type of autograft.
Transplants are performed in a sterile setting under the supervision of skilled medical professionals to reduce the risk of infection or complications. The need for immunosuppressive medications is lessened or even not required as the graft material is taken from the same person's body. Autografts take tissue from the same patient, which reduces the risk of rejection, unlike allografts, where the risk is increased due to harvested tissues originating from a different individual.
The autografted tissue originating from the same person integrates and functions better because of its biological compatibility. Autografts are a popular choice among doctors and patients due to their benefits. Autografts are an intriguing facet of contemporary medicine. They offer useful tools in the treatment and management of various medical conditions with a variety of applications, including bone grafts and stem cell transplants. The benefits autografts provide make them a desirable choice, despite the procedures' complexity.
What Is Autograft Tissue?
An autograft tissue is a surgically removed tissue from one location in a patient's body to another. The word “autograft” originates from the Greek words "auto" meaning self and "graft" meaning transplantation. Autografts take advantage of the individual's biological material to repair or replace damaged or diseased tissue.
Autograft tissue is highly compatible with the recipient's body, given that it is derived from the same individual. The body recognises autograft tissue as its own, which mitigates the risk of rejection commonly associated with transplants. Autografts encompass various types, such as skin, bone, and veins.
The autograft procedure involves a surgical operation. Taking skin from one part of the body, such as the thigh or buttock, to use in another part of the body is an example of skin graft harvesting. Dermatomes are used for the procedure. Dermatomes are specialised instruments that allow for the precise control of the depth and width of the skin being removed.
Orthopaedic surgeons opt for the iliac crest on the hip, the distal radius in the forearm, or the tibia's proximal portion for bone autografts. The specific site chosen depends on the quantity of bone needed and the patient's health. Various tools, such as osteotomes and curettes, are employed to remove the bone safely.
Soft tissue autografts, such as tendons and ligaments, require careful dissection and removal. An anterior cruciate ligament (ACL) reconstruction uses autografts, which are tendons or muscles from the patient's knee. Surgeons use surgical scissors, scalpels, and other dissection tools during the procedure.
Autograft tissue plays a significant role in various medical fields. Orthopaedic procedures involving spinal fusion or the enhancement of bone growth in the presence of a bone defect frequently make use of autograft bone. An autograft skin is used by dermatologists to treat severe burns or significant skin injuries. Vascular surgeries utilise autograft veins to serve as bypass grafts.
Autograft tissue serves as a valuable tool in the medical field, providing a biocompatible, low-risk option for tissue replacement or repair across various specialities.

How Does Autograft Tissue Work?
An autograft tissue works based on its biological compatibility. The patient’s immune system recognises autograft tissues without issue as they are derived from the patient itself. The recognition negates the risk of an immune reaction or rejection that is commonly associated with foreign transplants.
The autograft process begins with selecting a donor site. The donor site is the area in the patient's body where healthy tissue is available for extraction. The tissue from the donor area is surgically removed and transplanted to the recipient site. The recipient site is the area where repair or replacement is necessary.
The recipient site accepts the transplanted tissue. The body's natural healing processes integrate the graft with the surrounding tissue over time. Autograft tissues’ functions differ depending on the type of tissue involved.
An autograft bone gives new bone a place to grow and speeds up the healing process when it is put on a wound. An autograft skin aids in the formation of new skin and hastens the healing applied to a wound.
Autograft tissue is composed of the patient’s biological material. It encompasses various tissue types, ranging from skin, bone, and veins, to more specialised tissues, such as heart valves or corneas. Choosing which autograft tissue type to use is dependent on the condition that is being treated and the specific requirements of the recipient site.
An autograft skin is used in the treatment of severe burns. The skin is carefully harvested from an unburned area of the patient's body and transplanted to the burn site. Autograft bone is preferred for cases involving bone degeneration or loss.
Bone is taken from a site, such as the hip or tibia, and transplanted to the site of bone loss, providing a framework for new bone to grow. Autograft tissue leverages the body's resources to promote healing and recovery. Its composition is biocompatible as it is made of the patient's tissue. It minimises the risk of rejection and promotes a more natural integration with the surrounding tissue.
What Is the Main Purpose of Autograft Tissue?
The main purpose of autograft tissue lies in its use for the repair, reconstruction, or replacement of damaged or diseased tissues within the same individual's body. Autografts come from the patient’s body, which bypasses many compatibility issues faced with donor transplants.
Autograft tissue has extensive utility across various medical specialities. Autograft bone tissue is integral to procedures such as spinal fusion and bone defect repair to promote bone growth and solidify structural stability.
Anterior cruciate ligament reconstruction surgeries, such as the torn anterior cruciate ligament, depend on autograft ligaments that are taken from the patellar or hamstring tendon.
Bone autografts provide a natural scaffolding on which new bone cells grow, aiding in the healing process and facilitating the restoration of function.

Dermatologists use autograft skin for graft surgeries to treat skin damage resulting from severe burns or significant skin injuries. Autograft skin integrates with the surrounding tissue, which hastens the formation of new skin, accelerates the healing process, and improves the patient's recovery.
Vascular surgeons use autograft veins as bypass grafts. Vein autografts come from the patient’s legs. The primary goal is to reroute blood flow around blocked or damaged vessels, ensuring an uninterrupted supply of blood to vital organs.
Cosmetic surgeries incorporate autografts in various ways. Fat grafting is a common technique where fat is taken from one part of the body and injected into another.
The main purpose is to enhance aesthetic appeal by reshaping or augmenting areas including the face, buttocks, or breasts. Autografts are preferred due to the low risk of rejection and the natural appearance they impart.
Such cases highlight the purpose of autograft tissues, which is to aid the body's natural healing processes by providing compatible, biological material for the repair or replacement of damaged or lost tissues.
An autograft tissue serves another purpose, which is to reduce the risk of immune rejection and related complications. The risk reduction against rejection is due to the immune system’s recognition of the autograft tissue as “self,” as it comes from the patient itself.
Autograft tissue serves two purposes, with physical repair or replacement as the main one. Its secondary purpose is the promotion of healing, recovery, and the improvement of patient outcomes by reducing the risk of transplant-related complications.
How Is Autograft Tissue Applied in Dentistry?
Autograft tissue is applied in dentistry, such as in periodontal and oral-maxillofacial surgeries. Dental surgeons use autograft bones in grafting procedures involving bone defects resulting from trauma, disease, or developmental abnormalities.
Autograft bone tissue aids in bone generation. They are taken from the patient’s chin or the posterior part of the lower jaw.
Socket preservation is implemented following a tooth extraction. Autograft tissue assists in filling the empty socket to prevent bone loss and preserve the alveolar ridge for future implant placement. It serves as a scaffold, providing a structure on which new bone cells grow and proliferate.
Autograft tissue serves an important role in sinus lift procedures. The sinus floor needs to be elevated in certain cases to create enough bone height for dental implant placement. Autograft bone tissue from the patient gets used to augment the sinus floor and provide a solid base for the implant.
Periodontal regeneration procedures employ autografts to repair and regenerate the lost tissue. Patients with periodontal disease have damage to the gum and bone around the teeth. Autograft tissues used in periodontal regeneration procedures are connective tissue grafts taken from the roof of the mouth.
An autograft tissue provides a natural and compatible material that supports healing and regeneration. It offers several advantages, such as excellent biocompatibility, reduced risk of disease transmission, and a lower chance of rejection.
Autograft tissue is a valuable tool for dental surgeons, contributing to improved patient outcomes and enhanced quality of life.
What Are the Tissues Used for Autograft Tissue in Dentistry?
The tissues used for autografts are bone and soft tissue. An autograft bone tissue is sourced from the chin, the posterior part of the bottom jaw, or other non-oral locations, such as the hip or tibia. Soft tissue autografts are gingival and connective tissues harvested from the palate.
Autografted bone tissues provide a highly compatible material for bone grafting procedures. Autograft bone tissues address bone defects that occur as a result of trauma, disease, or developmental abnormalities. Soft tissue autografts help treat gum recessions, enhance the aesthetics of the gum line, or increase the bulk of soft tissue around dental implants.
Bone and soft tissue autografts contribute to function restoration and aesthetics, enhancing the oral health and quality of life for the patient. Autografts are entirely compatible with the patient's existing tissue since they are harvested from the patient itself. It eliminates the risk of an immune response or rejection.
Autografts carry no risk of transmitting infectious diseases, unlike other grafting procedures, such as allografts or xenografts, where graft tissues come from other individuals or species, respectively. Autografts possess the unique ability to integrate with the host bone, allowing for complete integration and remodelling over time.
Autograft tissues contain live cells and growth factors contributing to new bone formation and tissue regeneration. Autografted tissues promote faster and more robust healing. The benefits of autografts outweigh the drawbacks, such as the need for an additional surgical site, which introduces complexity and increases the risk of morbidity.
How Does Autograft Tissue Differ from Other Grafting Methods?
Autograft tissue holds distinctive attributes in comparison to other grafting methods in dentistry, such as allografts, xenografts, and alloplasts. Attributes include compatibility, risk of disease transmission and immunological reaction, and level of surgical invasiveness.
Autografts have the best compatibility and the least risk of disease transmission and immune reactions, as the tissue is being harvested from the patient itself. It contains viable cells, aiding in the regeneration and repair of the damaged area.
Autografts are deemed the gold standard against which other types of grafts are compared due to their benefits. Autografts are used in bone grafting procedures to ensure success. Allografts use tissues or cells from another individual of the same species, such as human-to-human transplants. Harvesting tissues from the same species reduces the risk of disease transmission but is not eliminated.
Allografts do not contain live cells, which makes regeneration and integration slower compared to autografts. Allografts have the benefit of not needing a second surgical site, which is required in autograft procedures. The lack of a second surgical site makes allografts less invasive and less painful for the patient.
Xenografts, derived from a different species, usually bovine or porcine, and alloplasts, which are synthetically manufactured, have a lesser risk of disease transmission. A xenograft tissue is processed to retain its structure, which aids in bone regeneration, but it lacks the presence of viable cells.
Alloplasts are comprised of biocompatible synthetic materials and have the advantage of being readily available. Alloplasts avoid the ethical issues associated with the use of human or animal tissues. Xenografts and alloplasts lack the superior integration and regenerative capabilities that autografts offer.
The best grafting method to use is chosen based on factors such as the specific clinical situation, patient preferences, availability of graft material, and the dentist's experience and comfort with the bone grafting procedure. Various types of autografts, allografts, xenografts, and alloplasts are used in the restoration and reconstruction of oral tissues, each with distinctive advantages and limitations.

How to Get an Autograft Tissue?
To get autograft tissue, follow the 7 steps listed below.
- Initiate a consultation. Set up a meeting with a dental specialist or oral surgeon to discuss the need for an autograft, understand the specific needs, and evaluate the health status.
- Perform diagnostic tests. Take part in diagnostic tests, such as X-rays, CT scans, or MRIs. X-rays, CT scans, or MRIs help to assess the areas in need of grafting and plan the autograft procedure.
- Determine the harvesting site. Work with the surgeon to identify the most suitable site for harvesting the autograft. Common sites for graft harvesting include the iliac crest, tibia, or intraoral sites such as the mandible or maxilla.
- Undergo the autograft procedure. Prepare for the autograft procedure. The process involves the surgeon removing a piece of tissue from the predetermined site and then grafting it onto the area in need.
- Participate in post-procedure care. Engage in recommended post-procedure care to ensure proper healing and graft integration, including taking prescribed medications, limiting certain activities, and attending follow-up appointments with the surgeon.
- Attend regular follow-up visits. Schedule and attend follow-up visits with the surgeon. Follow-up visits allow the surgeon to monitor healing progress, address any complications, and guide the next steps of the recovery process.
- Complete rehabilitation. Participate in any necessary rehabilitation, such as physical therapy or specific exercises, to regain function and promote optimal graft incorporation. The healthcare provider offers specific instructions tailored to individual recovery.

How to Manage Pain After Autograft Tissue Collection?
To manage pain after autograft tissue collection, there are guidelines to follow. Keep in constant communication with the doctor. Understanding the expected recovery timeline, the level of discomfort typically experienced, and the available pain management strategies help navigate the postoperative period. Clear communication with the healthcare provider is crucial to managing pain effectively.
Follow doctor prescriptions for medicines. Pain management is achieved through medications prescribed by the doctor. Patients receive the prescriptions before the procedure, allowing them to fill out the prescription and have the medication readily available after the procedure.
Use pain medication correctly. Pain medication must be taken correctly based on the guidelines set by the doctor to avoid overuse or potential dependency. Notify the doctor immediately if the prescribed medication does not adequately manage the pain or if it causes side effects.
Ensure the site is well-rested and elevated. Resting and elevating the donor site reduce swelling and discomfort. Gentle movement is recommended to prevent stiffness and promote blood flow, which aids in healing. Patients must avoid strenuous activities and movements that put stress on the harvested area. Alternating periods of rest with periods of gentle movement is recommended to ensure effective pain management.
Apply cold packs to the affected area. Cold pack application reduces inflammation and relieves pain. The cold pack must be wrapped in a cloth or towel to prevent skin damage and must not be applied for more than 20 minutes at a time.
Maintain good hygiene. Poor oral hygiene leads to an infection, causing more pain and complications. Gentle brushing, using mouthwash, and flossing after a dental autograft procedure help maintain a clean mouth and prevent infection.
Maintain good nutrition and hydration. Good nutrition and hydration play a significant role in healing and pain management. A balanced diet rich in protein, vitamins, and minerals promotes tissue repair and strengthens the immune system. Keeping hydrated aids in recovery and prevents constipation, a common side effect of some pain medications.
Adhere to follow-up appointments. Regular follow-up visits with the doctor ensure that the healing process is progressing well. Follow-up visits provide an opportunity to discuss any ongoing pain, concerns, or potential complications. The healthcare provider adjusts the pain management plan if necessary, based on the healing process and the patient's feedback.
How Is Autograft Tissue Compatibility Between Donor and Recipient Determined?
Autograft tissue compatibility depends on several factors, such as the patient’s health, anatomical similarity between the donor and recipient sites, and the condition of the donor and recipient sites.
Autografts offer high compatibility since the tissue is harvested from the patient itself but such factors still affect how well the patient’s body accepts the transplant. Good general health is beneficial in aiding recovery and successful integration of the graft.
Pre-existing conditions, such as diabetes or autoimmune diseases, need special consideration as they impact the healing process. The anatomical and physiological similarity between the donor and recipient sites is important. Graft integration and functionality increase if the sites have increased similarities.
Tissues harvested from the palate for use in the gum area have a high rate of success due to their anatomical and physiological similarities in dental grafting procedures. The condition of the donor site and recipient site influences the grafting’s success. The sites need to be free of infection or disease.
The recipient site must be prepared to receive the graft, and the donor site must be healthy enough to provide a viable graft and heal post-harvesting. Adequate post-procedure care at both sites has equal importance in ensuring the graft's success and minimising potential complications.
Autografts ensure immunological compatibility, but factors such as patient health, similarity between donor and recipient sites, and the condition of both sites are pivotal in ensuring graft compatibility.
Can the Recipient's Immune System Reject Autograft Tissue?
No, the recipient's immune system does not reject autograft tissue. The principle behind autografts lies in using the patient's tissue for transplantation The tissue from the patient’s body ensures the graft does not contain foreign antigens and the immune system does not recognise it as a threat.
Immunological rejection is minimised in autografts. Rejection is a concern in other grafting methods, including allografts, where tissue is derived from another person. Successful grafting is not guaranteed, despite the immune system's acceptance of the autograft.
Factors, such as the health status of the patient, the condition of the donor and recipient sites, and post-procedure care, influence the success of the graft. Proper handling of such aspects leads to a higher success rate in tissue grafting and ensures the recipient's recovery. Proper surgical and post-operative care is still crucial for a successful grafting procedure, even when the immune system does not reject the autograft.
What Are the Advantages of Using Autograft Tissue?
The advantages of using autograft tissue are listed below.
- Immune system compatibility: Autografts provide a high level of compatibility as tissues are taken from the patients themselves. They are recognised as “self” by the immune system, eliminating the risk of immune rejection. Self-recognition contributes to the successful incorporation of autografts into the recipient site.
- No disease transmission: Disease transmission from donor to recipient is a primary concern during transplants but is not a problem with autografts. Autografts harvest tissues from the patient itself, circumventing the risk of transmission of infectious diseases and making the procedure safer.
- High success rate: Autografts exhibit a higher success rate compared to other grafting methods, such as allografts or xenografts. The tissues from the same body allow them to integrate better with the surrounding tissue at the recipient site, facilitating a more successful and natural healing process.
- No donor required: Autograft procedures do not require finding a matching donor. It eliminates the issues associated with donor scarcity or the need for matching tissue types, as the donor and recipient are the same individuals.
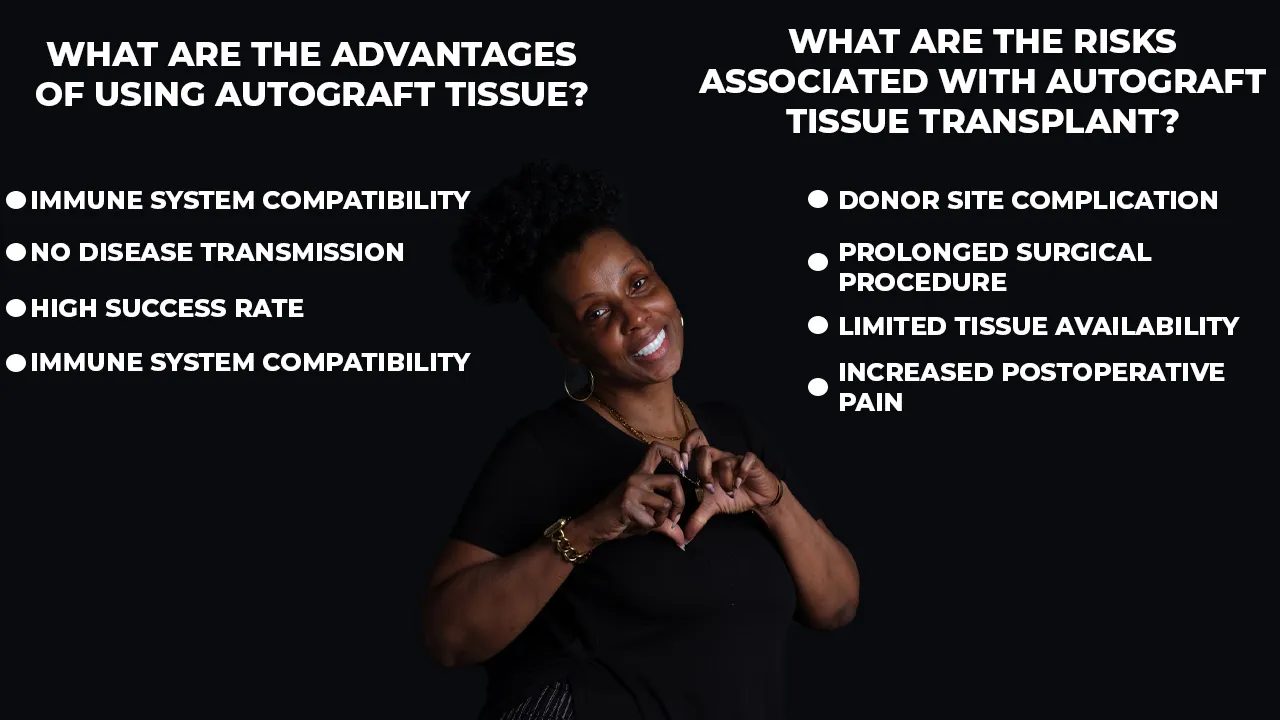
What Are the Risks Associated with Autograft Tissue Transplant?
The risks associated with autograft tissue transplants are listed below.
- Donor site complication: Autograft procedures necessitate an additional surgical site for tissue harvesting. The additional site presents a risk for complications, such as infection, increased pain, scarring, or impaired function at the donor site.
- Prolonged surgical procedure: The involvement of an additional surgical site in autograft procedures extends the duration of surgery. An extended procedure duration increases the risk of surgical complications, including infections.
- Limited tissue availability: The amount of autograft tissue available for harvest depends on patient specifics. Required tissue quantities in certain cases exceeding what is safely harvestable cause issues with the success of the grafting procedure.
- Increased postoperative pain: Patients undergoing autograft procedures experience increased postoperative pain due to the presence of two surgical sites. Pain management requires additional medications and extends recovery time.
What Are the Factors that Determine the Success of Autograft Tissue Transplant?
The factors that determine the success of autograft tissue transplants are listed below.
- Patient's General Health: The patient’s overall health affects the success of autograft transplants. Healthy patients have a better recovery rate and a lower risk of complications, leading to more successful outcomes.
- Tissue Harvesting Technique: The tissue harvesting technique impacts autograft transplants' success. Proper surgical technique ensures minimal damage to the harvested tissue, which increases the viability and success rate of the graft.
- Postoperative Care: Postoperative care influences the success of autograft tissue transplants. Regular monitoring, appropriate wound care, and early identification of complications help in the successful integration of the graft.
- Rehabilitation and Physical Therapy: A well-planned rehabilitation and physical therapy programme aids in restoring function and ensuring the long-term success of the graft.
- Site Preparation: Adequate preparation of the recipient site is vital for the success of the graft. Good blood supply and debridement of unhealthy tissue at the recipient site aid in graft incorporation and healing.
What Is the Success Rate of Autograft Tissue?
Autograft transplants have high success rates ranging from 85% to 90%, depending on the specific type of surgery involved. Bone autografts in implant dentistry have shown a 90% success rate, with autografts promoting bone formation and integration. Autografts have been the gold standard in orthopaedic surgeries for decades.
For example, anterior cruciate ligament (ACL) rebuilding procedures use autografts, with success rates exceeding 85%. Autografts have full compatibility with the patient’s body as they're sourced from the patient itself. The compatibility allows for greater success.
Ensuring factors such as health, surgical technique, and postoperative care are great ways to improve success rates. The success rate is high in autograft procedures but they are not devoid of challenges and complications. Risks include donor site morbidity, limited availability of graft material, and increased operative time.
Autografts continue to be accepted and have high success in various fields of medicine due to their excellent biological compatibility along with graft efficacy, despite the risks. Ongoing research aims to further mitigate the associated risks and improve the overall efficacy and patient experience of autograft procedures.
What Is the Typical Healing Process After Autograft Tissue Transplant?
The healing process after an autograft tissue transplant progresses through several phases, starting from the first day, and first week, to the first month and beyond. Each phase is marked by different physiological responses.
The body responds to the graft on the first day after the transplant. The body’s response focuses on managing inflammation and starting the healing process. Patients experience pain, swelling, and discomfort right after the surgery. Pain management is done through prescription analgesics at this stage.
The graft begins to stabilise as the week progresses. The body engages in removing damaged cells and debris from the site and starts the process of new vessel formation to supply blood to the site. Patients experience discomfort and swelling at this stage, but it starts to subside. Protecting the graft site from excessive stress and strain allows the healing process to be optimal.
The graft continues to integrate into the recipient site as the first month progresses. New tissue growth occurs as the body lays down collagen and other extracellular matrix components, forming a bridge between the graft and the surrounding native tissue. The body remodels the new tissue in the subsequent months, which enhances its strength and function.
Patients start resuming to perform more normal activities during these later stages. The timeline varies depending on the type of graft, the specific surgical procedure, and the individual patient's health and healing capacity.
Visual documentation can be extremely helpful during the autograft tissue transplant recovery process. Photos taken at regular intervals clearly illustrate changes from initial swelling and inflammation through to full integration and healing. These images provide patients with reassurance and understanding, enabling them to identify signs of healthy recovery or potential complications early on. Patients often find comfort and confidence in comparing their own experiences with professional bone graft healing photos.
How Long Does Autograft Tissue Take to Heal?
An autograph tissue takes several weeks to months to heal, depending on multiple factors. Factors include the type of graft used, the size and location of the graft, the patient's health, and the specific surgical technique employed.
The body starts to integrate the graft into the host site in the first weeks after surgery. Initial inflammation and discomfort start to diminish during this period. The body initiates the process of neovascularisation, the creation of new blood vessels to provide nutrients to the graft. The graft begins to stabilise at the recipient site during these early stages. The complete healing and integration of an autograft occur over several months.
Healing involves the remodelling of the new tissue, a process where the body enhances the strength and function of the graft. Complete recovery and return to full function take several months to over a year, depending on the specifics of the graft and the individual's healing capacity. Ongoing medical follow-ups throughout the healing process are crucial for tracking development and addressing any complications that arise.
Are Autografts Permanent?
Yes, autografts are permanent. Autografts’ permanence is due to the tissues being derived from the patient’s own body. Autografts sidestep the immune system's usual response to alien elements which enhances the longevity of the graft. The autograft integrates seamlessly into the body once the period of healing has concluded, replicating the role of the original tissue.
Autograft's permanence is highlighted in the treatment of extensive burns. Healthy skin, taken from an unaffected part of the same patient, is employed to cover burn wounds. The graft fosters healing by acting as a natural barrier for tissues beneath the surface. It merges with the surrounding tissue as time progresses, solidifying its position in the body permanently.
Autografts are permanent but still undergo alterations or adaptations over time as they are living tissues. Its permanence means its complete integration into the body, and it changes along the body over time. The main purpose of autografts is to facilitate repair and foster growth in the damaged area and that remains regardless of the changes they adapt over time.
What is an Example of Autograft Tissue Applied in Dentistry?
Dental implants are an example of autograft tissue applied in dentistry. Autografts aid in bone grafting procedures necessary to lay the groundwork for these implants. Bone grafts are necessary when an individual lacks the requisite bone quantity in the jaw before implant surgery.
Bone tissue from other parts of the individual's body gets harvested in dental bone autografts. Usual locations include the chin or posterior region of the lower jaw. Transplantation of the harvested bone to the required site in the jaw provides a stable base for the dental implant. The autograft integrates with the existing bone structure over time, becoming an integral and permanent part of the jaw.
Autograft tissue has proved instrumental in resolving dental challenges, particularly when dealing with bone deficiencies. The application of an autograft in such situations exhibits its versatility and effectiveness within the field of dentistry, solidifying its position as a reliable medical intervention.

Can Autograft Tissue Be Used in Reconstructive Surgery?
Yes, autograft tissue can be used in reconstructive surgery. The autograft serves a pivotal role in reconstructing damaged or lost tissues, providing a source of material that has a high likelihood of acceptance by the body. Autografts remain the preferred choice due to the minimised risk of rejection.
The body perceives autografts as “self,” reducing instances of an immune response. The integration of autograft tissue into the surgical site occurs naturally over time, eliminating concerns of rejection or adverse immune response. For instance, autograft tissue aids in reconstructing soft tissues during plastic surgeries.
Surgeons harvest skin from one body area to replace damaged or missing skin elsewhere. Skin autografts help treat severe burns or extensive wounds. Skin autografts help speed up recovery and minimise pain due to their high compatibility with the patient’s body. Orthopaedic surgeons use autografted bone tissues to treat and repair bone loss or defects.
Procedures, such as spinal fusion surgeries and bone reconstruction after trauma or cancer treatment, benefit from autografts due to their healing and growth factors. The advantage of autografted bone lies in its osteoinductive properties. It stimulates new bone growth and promotes healing and integration within the surgical site.
The tissue for these grafts comes from a different site on the patient's body, ensuring compatibility and facilitating recovery. The drawbacks include the extra surgical site, which means additional pain and the risk of complications. Autografts remain a robust tool in the arsenal of reconstructive surgery, despite the drawbacks. These characteristics highlight the importance and versatility of autograft tissue in reconstructive surgery.
What Are the Differences Between Autograft Tissue and Allograft Tissue?
The difference between autograft and allograft tissues is the source of the tissue. Autografts harvest tissue from the patient’s own body, while allografts harvest tissue from another individual. Autograft tissues are readily accepted by the patient’s body, making them a preferred choice in many surgical procedures.
Autografts avoid issues with rejection or any immune reactions that cause complications. Allograft tissues originate from a donor and are harvested post-mortem and then processed to ensure their safety before use. The allograft tissue being from another body increases the risk of rejection by the patient’s body if the immune system detects it as foreign and then attacks it. The immune reaction causes complications.
A key advantage of allografts is their availability in large quantities. Allografts are kept in tissue banks, which allows patients to proceed with the surgery in cases where there’s not enough viable tissue to be harvested from the patient. Another advantage of allografts is that they do not require secondary surgery for harvesting tissue from the patient, unlike autografts, where that is required.
The question "What is an allograft vs autograft?" asks which grafting method is better. The answer depends on the situation and what is deemed necessary by the doctor. The risk of rejection and disease transmission is one factor to consider. Autografts carry a minimal to zero risk of immunological rejection or disease transmission due to tissues being harvested from the patient’s own body.
Allografts have an increased risk for rejection and immune reactions due to the tissues being harvested from another individual, despite extensive screening and processing. Another consideration is the amount of tissue needed to repair the affected area.
Certain situations require large amounts of tissue. Allograft tissue is best suited for these cases since it is readily available through donors and tissue banks. Autografts and allografts have their advantages and are chosen based on the specific needs and constraints of each case.





